Wilson’s disease (Hepatolenticular Degeneration) is a rare genetic disorder where the body accumulates excessive copper due to a malfunction in copper metabolism. This leads to copper buildup in organs like the liver, brain, and cornea, causing various symptoms such as hepatic issues, neurological disturbances, and eye abnormalities. If left untreated, it can result in severe complications. Treatment involves copper-reducing medications and dietary adjustments to manage copper levels and alleviate symptoms.
Table of Contents
ToggleHow Common is Wilson's Disease?
Wilson’s disease is considered a rare disorder, and its prevalence varies among different populations. In general, it is estimated to occur in approximately 1 in 30,000 to 1 in 50,000 individuals worldwide. However, the prevalence can be higher in certain populations with a higher prevalence of carriers of the mutated gene responsible for the condition.
How Does Wilson's Disease Affect My Body?
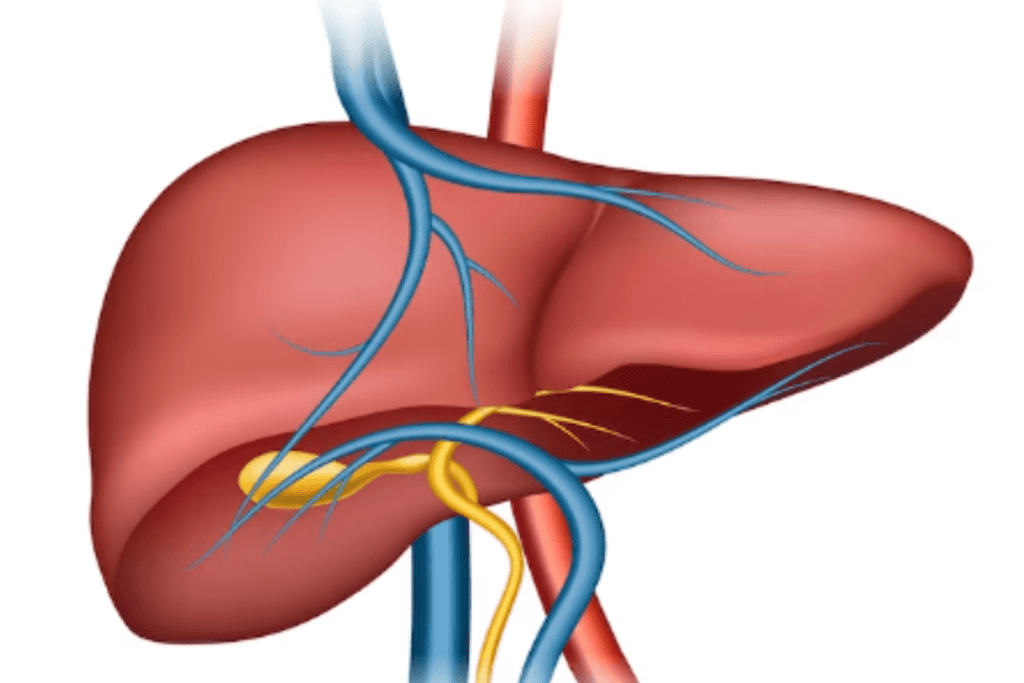
Wilson’s disease affects the body primarily by disrupting copper metabolism. Normally, the body excretes excess copper through bile, but in Wilson’s disease, this process is impaired. As a result, copper accumulates in various organs, particularly the liver, and brain, leading to damage over time.
In the liver, copper buildup can cause inflammation, scarring (cirrhosis), and impaired liver function. This can result in symptoms such as jaundice, abdominal pain, and fluid retention.
In the brain, the excess copper can lead to neurological symptoms like tremors, difficulty with fine motor control, muscle stiffness, and in severe cases, movement disorders similar to Parkinson’s disease. Cognitive and psychiatric issues, including mood swings, depression, and anxiety, can also occur due to brain involvement.
Other organs, such as the kidneys and cornea of the eyes, can also be affected by copper accumulation in Wilson’s disease.
What are the Symptoms of Wilson's Disease?
Wilson’s disease can manifest with a wide range of symptoms that vary in severity. The symptoms can be categorized into hepatic (liver-related), neurological, and psychiatric symptoms:
Hepatic Symptoms
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain or discomfort
- Enlarged liver and spleen
- Ascites (fluid buildup in the abdomen)
- Easy bruising and bleeding due to impaired clotting
- Fatigue and weakness
Neurological Symptoms
- Tremors or involuntary movements
- Difficulty with fine motor skills
- Muscle stiffness
- Dysarthria (speech difficulties)
- Difficulty swallowing
- Seizures
Psychiatric Symptoms
- Mood swings
- Depression and anxiety
- Irritability
- Personality changes
- Psychosis (hallucinations, delusions)
Some individuals might experience a combination of these symptoms, while others might have only one category of symptoms initially. Because the symptoms can be diverse and nonspecific, Wilson’s disease can sometimes be challenging to diagnose, especially in its early stages.
What Causes Wilson's Disease?
Wilson’s disease is caused by mutations in the ATP7B gene, which is responsible for producing a protein that plays a crucial role in transporting copper within the body. Normally, this protein helps transport excess copper from the liver into bile for elimination from the body. However, in individuals with Wilson’s disease, mutations in the ATP7B gene lead to a malfunctioning or absent copper transport protein.
As a result, copper cannot be properly excreted from the liver and ends up accumulating in various organs, particularly the liver and brain. This copper buildup leads to a wide range of symptoms associated with Wilson’s disease, including liver problems, neurological symptoms, and psychiatric disturbances.
Wilson’s disease is inherited in an autosomal recessive manner, meaning that a person must inherit two copies of the mutated gene (one from each parent) to develop the disorder. Carriers of a single mutated gene are usually asymptomatic but can pass the gene on to their children. When two carriers have a child together, there is a 25% chance that the child will inherit both mutated genes and develop Wilson’s disease.
How is Wilson's Disease Diagnosed?
Wilson’s disease can be challenging to diagnose due to its varied and sometimes nonspecific symptoms. A combination of clinical evaluation, medical history, and laboratory tests is typically used to diagnose the condition.
Here is a summary of the diagnostic procedure:
Clinical Evaluation
The doctor will assess your symptoms, medical history, and family history to determine if Wilson’s disease is a potential concern. Symptoms such as liver problems, neurological issues, and psychiatric symptoms might raise suspicion.
Blood Tests
Blood tests can help assess copper levels and the function of ceruloplasmin, a protein that carries copper in the blood. Low ceruloplasmin levels and elevated copper levels might indicate Wilson’s disease.
24-Hour Urine Collection
This examination quantifies the copper expelled in urine during 24 hours. Elevated levels of copper in the urine can indicate the presence of Wilson’s disease.
Liver Function Tests
These tests evaluate the liver’s health and function. Abnormal liver enzyme levels and other markers can indicate liver damage or dysfunction.
Genetic Testing
Genetic testing can identify mutations in the ATP7B gene, confirming a diagnosis of Wilson’s disease. However, not all individuals with Wilson’s disease have identifiable mutations on genetic testing.
Eye Examination
A slit lamp examination can reveal the presence of Kayser-Fleischer rings, which are copper deposits in the cornea of the eyes. These rings are a characteristic feature of Wilson’s disease.
Imaging Studies
Imaging techniques like ultrasound, MRI, or CT scans might be used to assess the liver and identify any signs of damage or abnormalities.
Liver Biopsy
In some cases, a liver biopsy might be performed to assess the extent of liver damage and copper accumulation.
How is Wilson's Disease Treated?
Wilson’s disease is a treatable condition, and with proper management, individuals with the disorder can lead relatively normal lives. The primary goal of treatment is to lower and maintain copper levels in the body to prevent further organ damage.
Treatment typically involves the following approaches:
Copper-Chelating Medications
Medications known as chelating agents are prescribed to help remove excess copper from the body. Commonly used chelating agents include D-penicillamine and trientine. These drugs bind to copper, allowing it to be excreted in the urine.
Zinc Supplementation
Zinc interferes with copper absorption in the digestive tract. By taking zinc supplements, individuals can reduce the amount of copper absorbed from their diet. This can be an effective long-term strategy to prevent copper accumulation.
Dietary Change
A low-copper diet might be recommended, although this is not the primary treatment method. Foods rich in copper, such as liver, shellfish, nuts, and chocolate, should be avoided or limited.
Regular Monitoring
Regular blood and urine tests are necessary to monitor copper levels and the effectiveness of treatment. Adjustments to medication dosages might be made based on these results.
Lifelong Treatment
Treatment for Wilson’s disease is usually lifelong. Once copper levels are under control, individuals often need to continue taking medications and following dietary guidelines to prevent relapses.
Liver Transplant
In cases where there is severe liver damage or failure, a liver transplant might be considered. This can effectively replace the damaged liver with a healthy one, resolving the issue of copper accumulation. However, this is usually reserved for cases where other treatments are ineffective or liver damage is advanced.
What Medications Treat Wilson's Disease?
Several medications are used to treat Wilson’s disease by helping to lower and maintain copper levels in the body. These medications work to chelate or bind to excess copper, allowing it to be excreted from the body.
The two main types of medications used for treating Wilson’s disease are:
D-Penicillamine
This medication is a chelating agent that binds to copper and helps remove it from the body through urine. It is one of the oldest and most commonly used treatments for Wilson’s disease. D-penicillamine can effectively lower copper levels and prevent further accumulation. However, it can have side effects, including skin rashes, gastrointestinal issues, and sometimes more serious reactions.
Trientine
Trientine is another chelating agent that works similarly to D-penicillamine. It is often used as an alternative treatment when individuals cannot tolerate D-penicillamine due to side effects. Trientine might have a lower risk of certain side effects but can still cause gastrointestinal issues.
Additionally, as part of the treatment plan, doctors might also recommend:
Zinc Supplementation
Zinc interferes with the absorption of copper in the intestines, reducing the amount of copper that enters the bloodstream. This can be an effective long-term strategy to prevent copper accumulation. Zinc supplements are usually taken with meals.
Vitamin B6 (Pyridoxine)
Some individuals with Wilson’s disease have a specific genetic mutation that impairs the metabolism of vitamin B6. In these cases, taking vitamin B6 supplements can improve the body’s ability to process and eliminate excess copper.
Are There Complications of Wilson's Disease Treatment?
While treatment for Wilson’s disease is generally effective in managing copper levels and preventing complications, there can be potential complications and side effects associated with the medications used to treat the condition.
It’s important to be aware of these potential issues and discuss them with your healthcare provider:
Medication Side Effects
The chelating agents used to treat Wilson’s disease, such as D-penicillamine and trientine, can cause a range of side effects. These may include skin rashes, gastrointestinal disturbances (nausea, vomiting, abdominal pain), and occasionally more serious reactions like bone marrow suppression or kidney problems. Regular monitoring of blood counts and kidney function is essential.
Allergic Reactions
Some individuals may experience allergic reactions to the medications, including skin rash, itching, fever, or more severe reactions. If any unusual symptoms occur, it’s important to contact a healthcare provider promptly.
Interaction with Other Medications
The medications used for Wilson’s disease treatment can interact with other drugs. It’s important to inform your healthcare provider about all medications, supplements, and over-the-counter drugs you are taking.
Zinc-Related Side Effects
Zinc supplements, which are often used to reduce copper absorption, can cause gastrointestinal discomfort, nausea, and vomiting. Taking zinc with food can help mitigate these effects.
Nutritional Deficiencies
Strict avoidance of high-copper foods might lead to deficiencies in certain nutrients. A balanced and varied diet with guidance from a healthcare provider or dietitian can help prevent this issue.
Long-Term Compliance
Treatment for Wilson’s disease is usually lifelong. Adhering to medications, dietary recommendations, and regular monitoring can be challenging for some individuals.
Relapses
Even with treatment, occasional relapses of elevated copper levels can occur. Regular monitoring and adherence to the treatment plan are important to catch and manage such situations promptly.
What are the Complications of Wilson's Disease?
Wilson’s disease, if left untreated or poorly managed, can lead to various complications due to the accumulation of copper in different organs. Complications can affect the liver, brain, and other systems in the body. Proper treatment and management can help prevent or minimize these complications.
Some potential complications of Wilson’s disease include:
1. Liver Complications
Cirrhosis:
The accumulation of copper in the liver can lead to scarring (fibrosis) and eventually cirrhosis, which is advanced liver damage. Cirrhosis can result in impaired liver function and its associated symptoms.
Liver Failure:
Severe and untreated Wilson’s disease can progress to liver failure, where the liver is no longer able to perform its vital functions.
2. Neurological Complications
Movement Disorders:
Copper buildup in the brain can lead to movement disorders such as tremors, dystonia (involuntary muscle contractions), and difficulty with fine motor skills.
Parkinsonism:
Some individuals with advanced Wilson’s disease might develop symptoms similar to Parkinson’s disease due to brain damage affecting movement control.
Cognitive and Psychiatric Symptoms:
Neurological complications can include cognitive decline, mood swings, depression, anxiety, and even psychosis.
3. Psychiatric Complications
Personality Changes:
Copper buildup in the brain can lead to alterations in personality, behavior, and emotional well-being.
Psychosis:
In severe cases, individuals might experience hallucinations, delusions, and other symptoms of psychosis.
4. Hematological Complications
Anemia and Thrombocytopenia:
Copper accumulation can affect blood cell production, leading to anemia (low red blood cell count) and thrombocytopenia (low platelet count), which can result in bleeding disorders.
5. Renal Complications
Kidney Damage:
Copper buildup can also affect kidney function and potentially lead to kidney damage.
6. Ocular Complications
Kayser-Fleischer Rings:
These are copper deposits that can accumulate in the cornea of the eyes. They are a characteristic feature of Wilson’s disease and can be identified through an eye examination.
7. Bone and Joint Complications
Osteoporosis:
In some cases, Wilson’s disease and its treatment can impact bone health and lead to a higher risk of osteoporosis.
Who’s at Risk for Wilson's Disease?
Wilson’s disease is a genetic disorder, meaning it is caused by mutations in specific genes that are passed down from parents to their children. As such, individuals who have a family history of Wilson’s disease are at an increased risk. Nevertheless, the presence of a family history does not guarantee the development of the disease in every individual.
The disorder is inherited in an autosomal recessive manner, which means that an individual must inherit two copies of the mutated gene (one from each parent) to develop Wilson’s disease.
Here are some key points about who is at risk for Wilson’s disease:
Family History
Individuals with a family history of Wilson’s disease are at a higher risk, especially if close relatives, such as siblings or parents, have been diagnosed with the disorder.
Carrier Parents
Even if both parents are carriers (heterozygous) for the mutated gene that causes Wilson’s disease, the likelihood of their child developing the disease is low unless both parents pass on their mutated gene copies.
Ethnic and Geographic Factors
While Wilson’s disease occurs worldwide, it has been reported with higher prevalence in certain populations, such as people of Eastern European, Mediterranean, or Indian descent.
Consanguinity
If there is a history of consanguineous (blood-related) marriages in a family, the risk of passing on two mutated gene copies can be increased.
Genetic Testing
Genetic testing can identify carriers of the mutated gene even if they don’t exhibit symptoms. This testing can be useful for family planning and counseling.
Spontaneous Mutations
In some cases, Wilson’s disease can occur without a family history if there is a spontaneous genetic mutation.
How can I Prevent Wilson's Disease?
Preventing Wilson’s disease is not always possible, as it is a genetic disorder that is inherited from parents who carry the mutated gene. However, there are steps you can take to manage the risk, ensure early detection, and effectively treat the condition if it is present:
Genetic Counseling
If you have a family history of Wilson’s disease or are concerned about the risk, consider undergoing genetic counseling. Genetic counselors can provide information about your risk of carrying the mutated gene and passing it on to your children.
Family Screening
If you have been diagnosed with Wilson’s disease or carry the mutated gene, it’s important to inform family members so they can consider genetic testing and early detection.
Prenatal Testing
If both parents are carriers of the mutated gene, prenatal testing can help determine whether the fetus has inherited two copies of the mutated gene, indicating a risk of Wilson’s disease.
Maintain Regular Health Check-ups
Regular medical check-ups can help detect any early signs or symptoms of Wilson’s disease. If you notice any unusual symptoms, such as unexplained liver problems or neurological changes, seek medical attention.
Awareness of Risk Factors
Be aware of the risk factors for Wilson’s disease, such as family history, ethnicity, and geographic origin. Understanding your risk can prompt you to seek appropriate medical advice and testing.
Healthy Lifestyle
While a healthy lifestyle won’t prevent Wilson’s disease, it can contribute to overall well-being. Consume a well-balanced diet, participate in consistent physical activity, and refrain from excessive alcohol intake.
Early Diagnosis and Treatment
If diagnosed with Wilson’s disease, early initiation of treatment can prevent complications and improve long-term outcomes. Adhere to the recommended treatment regimen, follow medication instructions accurately, and maintain scheduled check-up appointments.
Remember that Wilson’s disease is a rare condition, and most people will not need to take preventive measures. If you have concerns about Wilson’s disease based on family history or other factors, consult with a healthcare provider or genetic counselor for personalized guidance.
What Should I Avoid Eating with Wilson's Disease?
While there is no specific “Wilson’s disease diet,” individuals with Wilson’s disease are often advised to manage their copper intake to help prevent further accumulation of copper in the body. Here are some general dietary guidelines that can be followed to minimize copper intake:
High-Copper Foods
Avoid or limit foods that are high in copper content, such as:
Organ meats (liver, kidneys, etc.)
Shellfish (oysters, crabs, mussels)
Nuts and seeds
Chocolate and cocoa
Mushrooms
Legumes (beans, lentils, peas)
Avocado
Whole grains (oats, barley)
Copper-Rich Beverages
Limit consumption of copper-rich beverages, including some types of tap water and well water, which might have higher copper content.
Copper Cooking Utensils
Avoid cooking and storing acidic foods (tomatoes, citrus fruits, vinegar-based dishes) in copper pots and pans, as this can leach copper into the food.
Moderation
While it’s important to limit high-copper foods, you don’t need to completely eliminate all sources of copper from your diet. Consuming a variety of foods and maintaining a balanced diet is essential for overall health.
Discuss with a Dietitian
If you have Wilson’s disease, it’s advisable to consult with a registered dietitian or nutritionist who can provide personalized guidance on managing your diet. They can help you create a balanced eating plan that considers your nutritional needs and limitations.
Conclusion
Wilson’s disease, a rare genetic disorder, disrupts copper metabolism, leading to harmful accumulation in organs. Diagnosis relies on clinical evaluation, genetic testing, and blood/urine analysis. Treatment includes chelating medications, zinc supplementation, and dietary adjustments. Early intervention is crucial to prevent complications like liver damage, neurological issues, and psychiatric symptoms. While a specific diet isn’t mandated, avoiding high-copper foods helps manage copper intake. Genetic counseling, regular check-ups, and adherence to treatment plans play vital roles in effectively managing Wilson’s disease, promoting a better quality of life, and minimizing associated risks.
References
https://www.ncbi.nlm.nih.gov/books/NBK441990/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3375662/?tool=pubmed
https://www.mayoclinic.org/diseases-conditions/wilsons-disease/symptoms-causes/syc-20353251
https://rarediseases.org/rare-diseases/wilson-disease/
https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/wilson-disease/treatments.html
https://www.niddk.nih.gov/health-information/liver-disease/wilson-disease/treatment