Tooth infection symptoms refer to the observable signs and sensations that indicate the presence of an infection within a tooth or its surrounding tissues. These symptoms are the body’s response to the infection and are typically caused by bacterial invasion and subsequent inflammation.
Table of Contents
ToggleThese symptoms serve as important indicators for individuals to seek dental care and receive appropriate treatment to address the underlying infection and alleviate the associated pain and discomfort.
What is a Tooth Infection
A tooth infection, also known as a dental abscess, is a localized collection of pus that forms within or around a tooth. It is caused by a bacterial infection that enters the tooth or its surrounding tissues. The infection typically occurs as a result of dental decay, trauma to the tooth, or gum disease.
When bacteria enter the tooth, they can reach the inner layers, including the dental pulp, which contains blood vessels, nerves, and connective tissue. This leads to inflammation and infection of the pulp, resulting in symptoms such as severe toothache, sensitivity to hot or cold temperatures, swelling, and pus discharge.
If left untreated, a tooth infection can spread to the surrounding gums, jawbone, and even other parts of the body, potentially causing serious complications. Prompt diagnosis and treatment by a dental professional are crucial to address the infection, alleviate pain, and prevent further damage or spread of the infection.
Tooth Infection Symptoms
While tooth infection symptoms can vary from person to person, here are 20 potential signs and symptoms that may indicate a tooth infection:
1. Severe Toothache
A tooth infection typically causes sharp or throbbing pain in the affected tooth. The pain can be intense and persistent, making it difficult to ignore or perform regular activities.
Related: Tooth Pain (Toothache): Overview
2. Pain that Worsens with Biting or Applying Pressure
When you bite down or apply pressure to the infected tooth, it can cause increased pain. This occurs because the infection irritates the nerves and tissues surrounding the tooth.
3. Persistent, Throbbing Pain
The pain associated with a tooth infection is often described as throbbing or pulsating. It can continue for extended periods, even when not actively biting or applying pressure.
4. Sensitivity to Hot or Cold Temperatures
A common symptom of a tooth infection is increased sensitivity to hot or cold foods and beverages. Even slight temperature changes can trigger pain or discomfort in the affected tooth.
5. Swelling of the Face, Cheek, or Jaw
As the infection progresses, it can cause swelling in the surrounding facial tissues. The affected area may appear swollen, and puffy, and feel tender to the touch.

6. Redness and Tenderness Around the Affected Tooth
The gums and tissues around the infected tooth may become inflamed, resulting in redness and increased sensitivity. This can make it painful to brush or floss around the affected area.
7. Difficulty Opening the Mouth or Chewing
In severe cases, the swelling and pain from a tooth infection can make it difficult to open the mouth fully or chew food comfortably.
8. Gum Inflammation or Swelling
The gums near the infected tooth can become inflamed and swollen. They may appear red, puffy, and feel tender. This inflammation is a response to the infection.
9. Gum Tenderness or Pain
The infected tooth can cause gum tenderness or pain, especially when pressure is applied or when brushing the area.
10. Bad Breath or Unpleasant Taste in the Mouth
The bacterial infection in a tooth can lead to a foul odor in the breath and an unpleasant taste in the mouth that persists even with regular oral hygiene practices.
11. Pus or Discharge Around the Tooth or Gums
As the infection progresses, it can result in the formation of pus, which is a thick, yellowish, or whitish discharge. Pus may be visible around the infected tooth or gums.
12. Fever
In some cases, a tooth infection can cause a low-grade fever as the body’s immune system responds to the infection. A persistent fever may indicate a more severe infection.
13. Headache
The pain from a tooth infection can radiate to the head, leading to headaches, especially in the temples or behind the eyes.
14. Earache
The nerves associated with the teeth and ears are interconnected, so a tooth infection can cause referred pain to the ears, resulting in an earache.
15. Neck Pain or Stiffness
Swelling and inflammation from a tooth infection can sometimes cause pain or stiffness in the neck, especially on the affected side.
16. Swollen lymph Nodes in the Neck or Jaw Area
The body’s immune response to a tooth infection can lead to swollen lymph nodes in the neck or jaw area. The swollen glands can be sensitive when touched.
17. Fatigue or General Malaise
A tooth infection can cause a general feeling of fatigue or malaise due to the body’s efforts to fight off the infection.
18. Difficulty Sleeping due to Pain
The severe toothache associated with a tooth infection can make it challenging to sleep comfortably. The pain can be particularly noticeable when lying down.
19. Changes in Bite or Tooth Alignment
In some cases, a tooth infection can cause changes in the way the teeth align when biting or chewing. This can be due to swelling, pain, or shifting of the affected tooth.
20. Abscess Formation, Which May Feel Like a Bump or Pimple on the Gums
As the infection progresses, an abscess may form. An abscess appears as a bump or pimple on the gums near the infected tooth. It can be filled with pus and is often accompanied by severe pain.
Types of Tooth Infections
Different types of tooth infections can occur. Here are the common types:
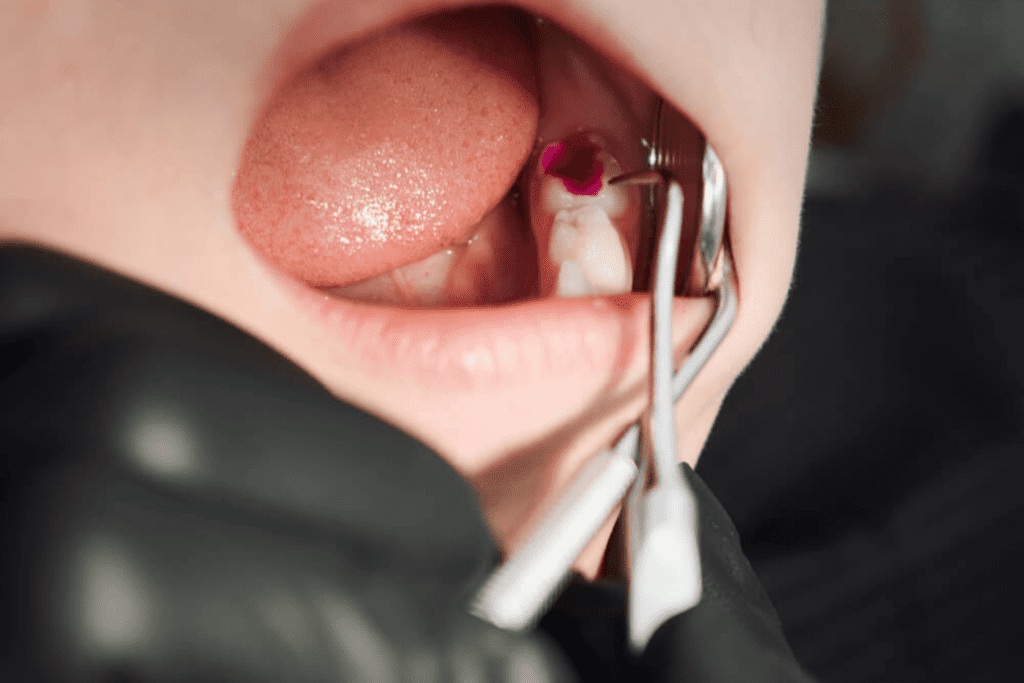
Dental Abscess
A dental abscess is a collection of pus that forms within the tooth or in the surrounding tissues. It is usually caused by a bacterial infection and can be categorized into two main types:
Related: Tooth Abscess
1. Periapical Abscess:
This type of abscess occurs at the tip of the tooth’s root. It usually develops as a result of untreated dental decay or dental trauma that has allowed bacteria to reach the pulp of the tooth.
2. Periodontal Abscess:
This abscess forms in the gums and is typically caused by an infection in the periodontal pocket, which is the space between the tooth and the gum. It is often associated with advanced gum disease (periodontitis).
Dental Fistula
A dental fistula, also known as a gum boil or gum abscess, is a channel that forms between an infected tooth or its root and the surface of the gums. It acts as a drainage pathway for an abscessed tooth. The fistula appears as a small pimple-like bump on the gum, and it can release pus or fluid.
Ludwig's Angina
Ludwig’s angina is a severe and potentially life-threatening infection that affects the floor of the mouth and the soft tissues of the neck. It usually starts as an infection in the lower molars and can rapidly spread, causing swelling, difficulty breathing, and potential airway obstruction.
Osteomyelitis
Osteomyelitis is a rare but serious infection that affects the bone of the jaw. It can occur as a complication of a dental infection, especially if left untreated or if the infection spreads. Symptoms include pain, swelling, and sometimes drainage of pus from the affected area.
Causes of Tooth Infection
Tooth infections, also known as dental abscesses, are primarily caused by bacteria entering the tooth or its surrounding tissues. Several factors can contribute to the development of tooth infection:
Dental Decay
Dental caries, or cavities, are the most common cause of tooth infections. When oral hygiene is insufficient, bacteria in the mouth produce acids that erode the tooth’s enamel, leading to decay. If left untreated, decay can progress deeper into the tooth, reaching the inner layers and causing an infection.

Poor Oral Hygiene
Inadequate brushing and flossing can allow plaque, a sticky film of bacteria, to accumulate on the teeth and gums. Over time, this can lead to tooth decay, gum disease, and an increased risk of tooth infections.
Dental Trauma
A tooth infection can occur as a result of dental trauma, such as a fracture, crack, or chip in the tooth. Trauma can expose the inner layers of the tooth, making it easier for bacteria to penetrate and cause an infection.
Failed Dental Procedures
In some cases, a tooth infection can develop as a result of a failed or incomplete dental procedure, such as a filling or root canal. If bacteria are not completely removed or the tooth is not adequately sealed, an infection can occur.
Gum Disease
Advanced gum disease, known as periodontitis, can lead to tooth infections. Gum disease causes inflammation and recession of the gums, creating pockets where bacteria can accumulate and cause infections.
Weakened Immune System
A weakened immune system due to certain medical conditions, medications, or treatments can increase the susceptibility to tooth infections. The immune system plays a crucial role in fighting off infections, including those in the teeth and gums.
Preexisting Dental Conditions
Existing dental conditions, such as enamel defects, tooth abnormalities, or malocclusion (misalignment of teeth), can make teeth more susceptible to decay and infections.
Impacted Wisdom Teeth
Wisdom teeth, also known as third molars, can become impacted or trapped beneath the gum line, making them difficult to clean properly. Impacted wisdom teeth can create pockets where bacteria can accumulate, leading to infection.
Signs of a Tooth Infection Extending to Other Parts of the Body
When a tooth infection is left untreated or becomes severe, there is a risk of the infection spreading beyond the tooth and affecting other parts of the body. This can lead to a condition called a dental or tooth infection spreading, which can have serious consequences. Here are some symptoms that may indicate a tooth infection spreading to the body:
Facial swelling
If the infection spreads, it can cause swelling not only in the immediate area around the affected tooth but also in the face and potentially the neck. The swelling may be accompanied by redness, warmth, and tenderness.
Difficulty Swallowing or Breathing
In rare cases, a severe tooth infection can spread to the deeper tissues of the face and throat, leading to difficulty swallowing or breathing. This situation demands urgent attention as it is a critical medical emergency.
Fatigue and Malaise
When an infection spreads, the body’s immune system is under stress, which can result in fatigue, weakness, and an overall feeling of being unwell.
Rapid Heartbeat
In some cases, an infection spreading from the tooth can cause an increased heart rate. This can occur due to the body’s response to the infection or if the infection reaches the bloodstream.
Swollen lymph Nodes
When a tooth infection spreads, it can cause the lymph nodes in the neck and jaw area to become swollen and tender. This is a sign that the body’s immune system is actively fighting the infection.
Headache
If the infection spreads to the sinuses or the tissues surrounding the brain, it can cause persistent headaches.
Dizziness or Lightheadedness
In severe cases, a spreading tooth infection can lead to systemic effects, including dizziness or a feeling of lightheadedness.
Nausea and Vomiting
Systemic infection can cause gastrointestinal symptoms such as nausea and vomiting.
Chest Pain or Difficulty Breathing
In rare instances, a severe infection can spread to the chest, causing symptoms such as chest pain, shortness of breath, or coughing.
If you experience any of these symptoms or suspect that a tooth infection may have spread, it is crucial to seek immediate medical attention. Dental or medical professionals can evaluate the situation, provide appropriate treatment, and prevent further complications.
How Does a Tooth Become Infected?
A tooth can become infected when bacteria enter the tooth structure or the surrounding tissues. The typical sequence entails the following steps:
Dental Decay
The most common cause of a tooth infection is dental decay, also known as a cavity. Decay occurs when the protective outer layer of the tooth, called enamel, is damaged by bacteria and acid produced by plaque. If not treated, decay progresses deeper into the tooth, reaching the softer inner layers.
Enamel Erosion
When dental decay progresses, it erodes through the enamel and reaches the underlying layer called dentin. Dentin is less resistant to decay and is more porous, allowing bacteria to penetrate more easily.
Infection of the Pulp
The innermost part of the tooth is called the pulp, which contains blood vessels, nerves, and connective tissue. If bacteria reach the pulp through a cavity, crack, or dental trauma, they can cause an infection. The pulp becomes inflamed and infected, leading to toothache and other symptoms.
Abscess Formation
As the infection progresses, the body’s immune response forms a localized collection of pus called an abscess. The abscess forms a defensive mechanism to contain the infection and prevent it from spreading further. The abscess can be located within the tooth (pulpal abscess) or at the root tip (periapical abscess).
Spread of Infection
If left untreated, the infection can spread beyond the tooth and into the surrounding tissues. The infection can extend into the gums, jawbone, or even the nearby facial structures. In severe cases, the infection can enter the bloodstream, causing systemic complications.
It’s important to note that tooth infections can also occur due to dental trauma, such as a fracture or break in the tooth, which allows bacteria to enter the inner layers. Additionally, poor oral hygiene, compromised immune systems, and certain medical conditions can increase the risk of tooth infections.
Conclusion
Tooth infections, also known as dental abscesses, can cause significant pain and discomfort if left untreated. They are primarily caused by bacteria entering the tooth or its surrounding tissues. Factors such as dental decay, poor oral hygiene, dental trauma, gum disease, and weakened immune systems can contribute to the development of tooth infections.
Recognizing the symptoms of a tooth infection, such as severe toothache, swelling, sensitivity, and pus discharge, is important for prompt diagnosis and treatment. Dental professionals can provide appropriate care to address the infection, alleviate pain, and prevent further complications.
Maintaining good oral hygiene practices, including regular brushing and flossing, along with routine dental check-ups, is essential for preventing tooth decay and infections. Addressing dental issues promptly and receiving proper dental care can help avoid the development of tooth infections.
If you suspect a tooth infection or are experiencing symptoms associated with it, it is crucial to seek dental care as soon as possible. Dentists can diagnose the condition accurately and provide appropriate treatment to restore oral health and prevent the infection from spreading to other parts of the body. Remember, early intervention is key in managing tooth infections effectively.
Resources
Image Designed by Freepik
References
https://www.ncbi.nlm.nih.gov/books/NBK542165/
https://www.mayoclinic.org/diseases-conditions/tooth-abscess/symptoms-causes/syc-20350901
https://www.ncbi.nlm.nih.gov/books/NBK493149/
https://www.nhsinform.scot/illnesses-and-conditions/mouth/dental-abscess