We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer

What is Root Canal Treatment?
Root canal treatment, also known as endodontic therapy, is a dental procedure performed to save a severely infected or decayed tooth. It involves removing the infected pulp tissue, which contains nerves and blood vessels, from the tooth’s root canal system. The process begins with the dentist numbing the area and creating an access point to reach the pulp chamber. The infected pulp is carefully cleaned and shaped, and the canals are filled with a biocompatible material. Finally, a crown or filling is placed on the tooth to restore its strength and functionality. The endodontic treatment alleviates pain, prevents further infection, and allows the natural tooth to be preserved.
Table of Contents
ToggleSigns and Symptoms of a Root Canal
Several signs may indicate the need for a root canal treatment:
Persistent Toothache
A severe and persistent toothache is often an indicative symptom of an underlying endodontic issue. The pain associated with it can vary, presenting as throbbing, sharp, or constant, and it may exacerbate when biting down or exerting pressure on the affected tooth. Such persistent discomfort is commonly associated with infection or inflammation within the tooth’s pulp, necessitating further evaluation and potential root canal treatment.
Sensitivity to Hot and Cold
If you experience heightened sensitivity to hot and cold temperatures that lingers even after the stimulus is removed, it could be a sign that the nerves within the tooth are affected. This sensitivity occurs because the damaged or infected pulp is unable to protect the nerves from extreme temperature changes.
Gum Swelling and Tenderness
Swollen and tender gums around a specific tooth can be an indication of an infected root canal. The infection within the tooth can spread to the surrounding gum tissue, leading to localized inflammation and tenderness.
Darkened Tooth
Discoloration or darkening of a tooth may signify that the pulp inside is damaged or dead. The tooth may appear grayish, yellowish, or even black. This discoloration occurs when the blood vessels within the tooth’s pulp are compromised due to infection or trauma.
Prolonged Sensitivity to Pressure
If a tooth remains sensitive to touch or pressure for an extended period, it could be a sign that the endodontic system is compromised. Inflamed or infected pulp can cause heightened sensitivity, making it uncomfortable to chew or apply any pressure on the affected tooth.
Presence of a Dental Abscess
A dental abscess is a pocket of pus that forms around the tooth’s root due to an infection. It often presents as a pimple-like swelling on the gums, accompanied by pain and sometimes an unpleasant taste in the mouth. An abscess is a serious condition and requires immediate dental attention, as it can lead to further complications if left untreated.
What Causes Root Canal?
Root canals are typically caused by the presence of infection or inflammation in the tooth’s pulp, which is the soft inner tissue containing nerves, blood vessels, and connective tissue. The following are common causes of endodontic problems:
Deep Tooth Decay
When tooth decay (cavities) is left untreated, bacteria gradually eat away at the outer layers of the tooth, reaching the inner pulp. The bacteria invade the pulp chamber and can cause infection and inflammation. As the infection progresses, it can lead to pain, sensitivity, and ultimately the need for a root canal treatment. Endodontic therapy is necessary to remove the infected pulp and prevent the spread of infection.
Dental Trauma
A severe blow or injury to a tooth can cause trauma to the pulp. Even if there are no visible cracks or fractures, the impact can disrupt the blood supply to the pulp, leading to tissue damage and eventually pulp death. The compromised pulp becomes susceptible to bacterial infection, necessitating a root canal procedure to clean and disinfect the endodontic system.
Dental Procedures
Repeated dental procedures on a tooth, such as multiple fillings, extensive drilling, or other interventions, can weaken the tooth’s structure and compromise the health of the pulp. These procedures can irritate the pulp, causing inflammation and infection. In such cases, a root canal may be needed to remove the damaged or infected pulp and restore the tooth’s health.
Cracked or Fractured Tooth
A cracked or fractured tooth can create a pathway for bacteria to enter the pulp. Cracks can occur due to various reasons, including biting on hard objects, trauma, teeth grinding (bruxism), or natural wear and tear. When the crack extends to the pulp, bacteria can infiltrate the pulp chamber, leading to infection and inflammation. To save the tooth and prevent further damage, a root canal treatment is often necessary.
Faulty Dental Restorations
Poorly fitted dental fillings or crowns can create gaps or openings between the restoration and the tooth structure. These gaps allow bacteria to seep in and contaminate the pulp, leading to infection. When an infection occurs, a root canal may be required to remove the infected pulp and restore the tooth’s functionality.
Dental Abscess
A dental abscess is a pocket of pus that forms at the root of a tooth. It usually develops as a result of untreated tooth decay, severe infection, or trauma to the tooth. The abscess can cause significant damage to the pulp, leading to infection and inflammation. Root canal treatment is often necessary to remove the infected pulp, eliminate the abscess, and save the tooth from extraction.
Related: Tooth Abscess
Types of Root Canal Treatment
There are different types of root canal treatments available depending on the complexity of the tooth’s anatomy and the specific requirements of the case. The main types of root canal treatment include:
Conventional Root Canal Treatment
This is the most common type of endodontic procedure. It involves accessing the tooth’s pulp chamber, cleaning and disinfecting the root canals, and then filling them with a biocompatible material called gutta-percha. Afterward, a dental crown or filling is placed on the tooth to restore its structure and functionality.
Endodontic Retreatment
In some cases, a previously treated tooth may develop a new infection or inflammation. Endodontic retreatment involves reopening the tooth, removing the existing filling material, and thoroughly cleaning and disinfecting the canals. The canals are then filled again with fresh gutta-percha. This procedure is typically performed when there are persistent symptoms or signs of root canal failure.
Apicoectomy
Also known as a root-end resection, an apicoectomy is a surgical procedure performed when conventional root canal treatment is not sufficient. It is done when there are persistent infections or issues with the tooth’s root tip (apex). During the procedure, the infected or inflamed tissue is removed, and the root tip is sealed to prevent further infection.
Pulpotomy
A pulpotomy is a partial root canal treatment primarily performed in children. It involves removing the infected pulp tissue in the crown portion of the tooth while leaving the vital pulp in the root canals intact. The canals are then filled with medicated material to promote healing. This procedure is usually done on primary (baby) teeth to preserve them until they naturally fall out.
Regenerative Endodontics
This is an emerging field in endodontics that aims to restore the functionality and vitality of damaged dental pulp. Regenerative endodontic procedures involve disinfecting the endodontic system, introducing bioactive materials, such as growth factors or stem cells, to encourage tissue regeneration, and sealing the tooth to prevent reinfection.
Steps and Stages of Root Canal Procedure
The endodontic procedure consists of several steps and stages to effectively treat an infected or damaged tooth. The typical steps and stages involved in a root canal procedure are as follows:
Examination and Diagnosis
The dentist examines the tooth, reviews dental X-rays, and evaluates the symptoms to diagnose the need for an endodontic procedure. The extent of infection or damage is assessed.
Local Anesthesia
Before commencing the procedure, the dentist carefully administers local anesthesia to the tooth and its surrounding area. This step is essential to effectively numb the area and ensure the patient’s utmost comfort and freedom from pain throughout the procedure.
Isolation

A dental dam, a thin sheet of rubber, is placed around the tooth being treated. This isolates the tooth from the rest of the mouth, providing a sterile working environment and preventing contamination.
Access Opening
Using specialized dental instruments, the dentist creates an access opening on the tooth’s surface. This involves drilling a small hole through the tooth’s crown, providing access to the pulp chamber and root canals.
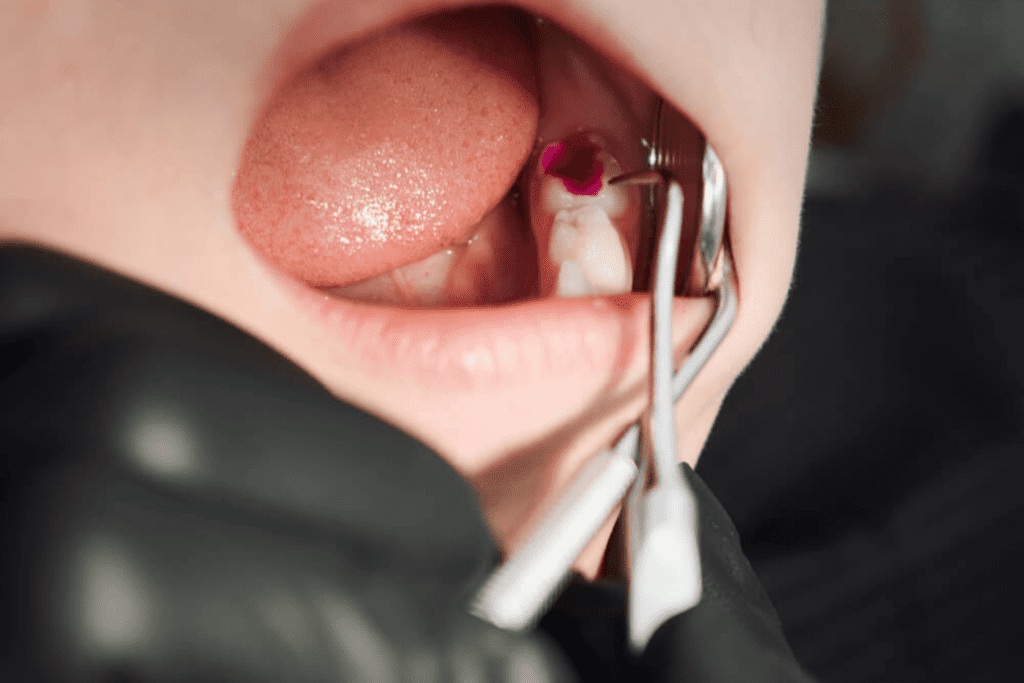
Pulp Removal (Pulpectomy)
The infected or damaged pulp inside the tooth’s pulp chamber and root canals is carefully removed using dental files. The dentist cleans and shapes the canals to remove any debris, bacteria, or infected tissue.
Irrigation and Disinfection
The root canals are irrigated with a disinfecting solution, such as sodium hypochlorite, to thoroughly clean and disinfect them. This helps flush out any remaining bacteria and disinfect the canals.
Obturation (Filling of Root Canals)
Once the canals have been thoroughly cleaned and shaped, they are filled with a biocompatible material known as gutta-percha. The dentist carefully inserts the gutta-percha into the canals and seals it with a specialized sealer to create a tight and effective barrier, preventing any potential recontamination. This crucial step guarantees the proper sealing of the root canal system, ensuring the success and long-term stability of the treatment.
Temporary Filling
A temporary filling material is placed in the access opening to protect the root canal filling and seal the tooth temporarily until a permanent restoration can be placed.
Restoration
In most cases, a dental crown is recommended to restore the tooth’s appearance, strength, and functionality. The crown is typically placed during a separate appointment after the endodontic procedure to protect the tooth from further damage.
Follow-up
The dentist may schedule a follow-up appointment to monitor the tooth’s healing and evaluate the success of the endodontic procedure. This may involve taking dental X-rays to assess the root canal filling and confirm the elimination of infection.
Why Do Dentists Always Recommend Root Canals?

Dentists recommend root canals when the pulp inside a tooth becomes infected, inflamed, or damaged beyond repair. Here are some reasons why dentists often recommend root canal treatment:
Infection Control
Root canal treatment is recommended when the dental pulp inside the tooth becomes infected or inflamed. This can occur due to deep cavities, tooth decay, or dental trauma that exposes the pulp to bacteria. By performing a root canal, the dentist can access the infected pulp, remove it, and thoroughly clean and disinfect the root canals. This process helps eliminate the infection and prevents it from spreading to the surrounding tissues, which can lead to more severe complications.
Pain Relief
Infected or damaged dental pulp can cause severe toothache and discomfort. The pulp contains nerves that can become inflamed and sensitive when infected. Root canal treatment involves removing the infected pulp, including the nerves, which provides immediate relief from persistent tooth pain. Once the infected pulp is removed, the tooth is no longer a source of pain for the patient.
Preservation of Natural Tooth
Dentists prioritize saving natural teeth whenever possible because they are the best option for function, aesthetics, and long-term oral health. Root canal treatment allows the dentist to save a tooth that would otherwise require extraction. By removing the infected pulp, cleaning and shaping the root canals, and sealing them with filling material, the tooth can be preserved and restored to its function and appearance.
Functionality and Chewing Ability
A tooth that has undergone root canal treatment, along with the placement of a dental crown, can regain its functionality. The dental crown acts as a protective cap that restores the strength and structure of the treated tooth. With a restored tooth, patients can resume normal chewing and biting activities without discomfort or limitations, ensuring proper digestion and oral function.
Prevention of Tooth Loss
If an infected tooth is left untreated, the infection can progress and weaken the tooth’s structure, potentially leading to tooth loss. Root canal treatment is performed to save the natural tooth, preventing the need for extraction. By eliminating the infection and restoring the tooth, the dentist can help patients maintain a full set of natural teeth, preserving oral health and preventing the complications associated with missing teeth, such as shifting of neighboring teeth or jawbone deterioration.
Aesthetics
After root canal treatment, the affected tooth is typically restored with a dental crown. The dental crown is custom-made to match the color, shape, and size of the surrounding teeth, ensuring a seamless and natural appearance. By restoring the tooth’s aesthetics, root canal treatment helps patients maintain a confident and attractive smile.
Cost-Effective
In the long run, root canal treatment can be a cost-effective option compared to tooth extraction followed by tooth replacement alternatives like dental implants or bridges. By saving the natural tooth through root canal treatment, patients avoid the need for more extensive and costly procedures. Additionally, preserving the natural tooth helps maintain the alignment and stability of neighboring teeth, reducing the risk of additional dental problems that may require further treatment and expenses.
Who is Not Eligible for a Root Canal Procedure?
While endodontic procedures are commonly performed to treat dental infections and save teeth, there are certain situations where a person may not be eligible for a root canal procedure. These situations include:
Irreparable Tooth Damage
If a tooth is severely damaged beyond repair, such as in cases of extensive tooth fracture or vertical root fracture, a root canal may not be a viable option. In these situations, the tooth’s structural integrity may be compromised to such an extent that it cannot be saved through root canal treatment. Tooth extraction may be necessary to prevent further complications and explore alternative tooth replacement options.
Advanced Gum Disease
Advanced gum disease, known as periodontitis, can lead to significant bone loss and compromised tooth stability. If the tooth affected by the infection is surrounded by severe gum disease, an endodontic procedure may not be feasible. The underlying gum disease needs to be addressed and controlled before considering any restorative dental treatment. In such cases, the dentist may recommend tooth extraction as part of the overall periodontal treatment plan.
Insufficient Tooth Structure
In some cases, a tooth may have insufficient healthy tooth structure remaining to support a successful endodontic procedure. This can occur when a large portion of the tooth has been destroyed by extensive decay, trauma, or previous dental treatments. If there is not enough sound tooth structure to retain a crown or provide adequate support for the tooth after root canal treatment, the tooth may not be eligible for the procedure. Tooth extraction and tooth replacement options, such as dental implants or bridges, may be considered instead.
Unrestorable Root Canal Anatomy
The root canal anatomy of a tooth can vary from person to person, and in some cases, it can present challenges that make the endodontic procedure highly complex or unpredictable. For example, if the root canals are unusually curved, narrow, or have complex branching patterns, it may be difficult for the dentist to thoroughly clean, disinfect, and seal them during the endodontic procedure. In such situations, the success of the root canal treatment may be compromised, and the dentist may recommend tooth extraction as a more reliable solution.
General Health Concerns
In certain instances, individuals with compromised immune systems, uncontrolled diabetes, or specific medical conditions that make them susceptible to infections may not be ideal candidates for an endodontic procedure. These conditions can impair the body’s ability to heal properly and increase the risk of complications. The dentist may explore alternative treatment options or consider tooth extraction in consultation with the patient’s healthcare provider to ensure the best possible outcome for the patient’s overall health.
How to Avoid Root Canal?

While it is not always possible to completely avoid the need for a root canal, there are several measures you can take to reduce the risk of developing severe dental infections or damage that may require an endodontic procedure. Here are some tips to help maintain good oral health and potentially minimize the need for a root canal:
Practice Good Oral Hygiene
Maintain a consistent oral hygiene routine by brushing your teeth at least twice a day using fluoride toothpaste and ensuring daily flossing. These practices help promote optimal dental health and hygiene. Good oral hygiene helps remove plaque, bacteria, and food particles that can contribute to tooth decay and gum disease. By keeping your teeth and gums healthy, you can lower the risk of infections that may necessitate a root canal.
Visit Your Dentist Regularly
Make it a habit to schedule regular dental check-ups and cleanings every six months or as advised by your dentist. These routine visits are crucial for maintaining optimal oral health and detecting any potential issues early on. By staying proactive with your dental care, you can minimize the chances of developing conditions that may require root canal treatment. Regular dental visits allow your dentist to detect any early signs of tooth decay, gum disease, or other oral health issues. Early intervention can help prevent these problems from progressing to the point of needing a root canal.
Address Dental Issues Promptly
If you experience tooth sensitivity, pain, or any dental problems, do not ignore them. Promptly visit your dentist to have the issue assessed and treated. Early intervention can often prevent minor dental issues from worsening and potentially requiring root canal treatment.
Maintain a Healthy Diet
To promote dental health and reduce the risk of dental issues that may necessitate root canal treatment, it is advised to limit the consumption of sugary and acidic foods and beverages. Instead, focus on maintaining a balanced diet that includes ample fruits, vegetables, whole grains, and lean proteins. A healthy and nutritious diet supports overall oral health and helps prevent tooth decay, reducing the likelihood of requiring root canal treatment.
Wear Protective Gear for Sports
If you participate in contact sports or activities with a risk of dental trauma, wear a mouth guard. Mouth guards help protect your teeth from injuries that can lead to cracked or fractured teeth, reducing the likelihood of needing a root canal due to trauma.
Avoid Using Teeth as Tools
Refrain from using your teeth to open packages, bite nails, or chew on non-food items. These habits can cause tooth fractures or damage that may require a root canal to restore the tooth’s function and structure.
Seek Professional Dental Care for Bruxism
If you grind or clench your teeth (bruxism), consult your dentist. They may recommend wearing a nightguard to protect your teeth from excessive wear and damage. Addressing bruxism can help prevent tooth damage that could potentially lead to a root canal.
Benefits of Root Canal
Root canal treatment offers several benefits for patients with infected or damaged teeth. Here are the key advantages of undergoing an endodontic procedure:
Elimination of Infection
Root canal treatment focuses on removing the infected or inflamed pulp tissue inside the tooth. By thoroughly cleaning and disinfecting the root canals, the dentist eliminates the source of infection. This prevents the bacteria from spreading further and causing more extensive damage to the tooth or surrounding tissues.
Pain Relief
Dental infections can be extremely painful, often causing severe toothaches and sensitivity to hot or cold temperatures. Root canal treatment provides significant pain relief by removing the infected pulp and relieving the pressure inside the tooth. Once the infection is eliminated, patients typically experience relief from the persistent toothache, allowing them to resume their daily activities without discomfort.
Preservation of Natural Tooth
One of the primary advantages of root canal treatment is the preservation of the natural tooth. Rather than extracting the infected tooth, the dentist removes the infected pulp and restores the tooth’s structure. Preserving the natural tooth is beneficial for several reasons. It maintains the natural appearance, function, and alignment of the teeth, ensuring a more natural and seamless smile. Additionally, it avoids the need for more extensive tooth replacement options, such as dental implants or bridges, which can be more invasive and costly.
Efficient Chewing and Normal Bite
After a successful endodontic procedure, the tooth is typically restored with a dental crown or filling. This restoration allows the tooth to regain its strength and functionality. Patients can chew and bite with the treated tooth just like they would with their natural teeth. Restoring the tooth’s structure and function allows individuals to enjoy their favorite foods without discomfort or limitations, contributing to improved overall oral function.
Aesthetics and Confidence
Root canal treatment, combined with a dental crown or filling, restores the appearance of the affected tooth. The dental restoration is designed to match the natural color and shape of the surrounding teeth, ensuring a harmonious and aesthetically pleasing smile. Having a healthy and restored tooth can significantly boost self-confidence and improve the overall appearance of the smile.
Prevents Jawbone Deterioration
If an infected tooth is left untreated, the infection can spread to the surrounding jawbone, leading to bone loss and deterioration. Root canal treatment removes the infection and preserves the tooth, which helps maintain the integrity and strength of the jawbone. By preventing further bone loss, root canal treatment contributes to the long-term stability and health of the jawbone.
Efficient and Cost-Effective
Root canal treatment is an efficient and cost-effective solution compared to tooth extraction followed by tooth replacement options like dental implants or bridges. The process of removing a tooth and pursuing alternative treatments can be more time-consuming, involve multiple procedures, and may require additional healing time. Root canal treatment allows patients to retain their natural teeth, avoiding the potential challenges and adjustments associated with tooth replacement.
Root Canal Treatment Risk and Side Effects

Like any medical or dental procedure, root canal treatment carries certain risks and potential side effects. However, it’s important to note that complications are relatively rare, and the benefits of root canal treatment typically outweigh the risks. Here are some potential risks and side effects associated with root canal treatment:
Discomfort and Sensitivity
Following an endodontic procedure, it is normal to experience some discomfort, sensitivity, or mild pain in the treated tooth and surrounding area. This can be due to inflammation of the tissues during the procedure or temporary irritation from the dental instruments. The discomfort is typically manageable with over-the-counter pain relievers and should subside within a few days as the healing process progresses.
Infection
The primary goal of root canal treatment is to eliminate infection from the tooth. However, there is a slight risk of persistent or recurring infection. This can happen if the entire infected tissue or bacteria are not completely removed during the procedure, or if there are additional undetected canals in the tooth. If the infection persists or returns, further treatment, such as retreatment or apicoectomy (surgical removal of the tooth’s root tip), may be necessary to resolve the infection.
Damage to Surrounding Structures
During the endodontic procedure, there is a minimal risk of damage to the surrounding tissues, such as the gums, nerves, or blood vessels. The dentist takes precautions to minimize such risks, but in rare cases, accidental damage can occur. Any potential damage is usually temporary and resolves with proper care and healing.
Fracture of the Tooth
Teeth that require root canal treatment are often weakened due to extensive decay, trauma, or previous dental work. As a result, there is a small risk of tooth fracture during or after the procedure. To protect the tooth and restore its strength, a dental crown is typically recommended. The crown covers and reinforces the treated tooth, reducing the risk of fracture and improving its long-term prognosis.
Failure of Treatment
While root canal treatment is highly successful, there is a small chance that it may not completely resolve the infection or eliminate the symptoms. Factors that can contribute to treatment failure include complex root canal anatomy, missed canals, or persistent bacteria. If the infection persists or symptoms persist, additional procedures, such as retreatment or apicoectomy, may be necessary to address the underlying issue.
Allergic Reactions
Although rare, some individuals may have an allergic reaction to the materials used during the root canal procedure, such as local anesthesia or filling materials. It is important to inform your dentist about any known allergies or sensitivities before the procedure to ensure appropriate alternatives or precautions are taken to avoid any adverse reactions.
Dental Treatment Alternatives to a Root Canal
When an endodontic procedure is not a viable option or is not recommended, there are alternative dental treatments available. The choice of alternative treatment depends on the specific circumstances and condition of the affected tooth. Here are several frequently considered alternatives to undergoing a root canal procedure:
Tooth Extraction
Tooth extraction involves the complete removal of the affected tooth from its socket in the jawbone. It may be recommended when the tooth is severely damaged, infected, or structurally compromised to the point where it cannot be saved through root canal treatment. Tooth extraction eliminates the source of infection and provides immediate relief from pain. However, it leaves a gap in the mouth that requires further consideration for tooth replacement options.
Dental Bridge
A dental bridge is a type of fixed dental restoration that serves as an alternative for replacing one or more missing teeth. It consists of dental crowns placed on the neighboring teeth (abutment teeth) with an artificial tooth (pontic) in between. The dental bridge fills the gap left by the extracted tooth, restoring both function and appearance. The abutment teeth need to be reshaped to accommodate the crowns, which can be a disadvantage if they are healthy teeth. Dental bridges are a non-removable option that provides stability and improved chewing ability.
Dental Implant
A dental implant is a highly effective and long-lasting alternative for replacing a missing tooth. It involves the surgical placement of a titanium implant into the jawbone, which serves as an artificial tooth root. After a healing period of a few months, a dental crown is attached to the implant, providing a natural-looking and functional replacement tooth. Dental implants offer stability, durability, and a more independent tooth replacement solution without relying on adjacent teeth. They mimic the look and function of natural teeth and can last a lifetime with proper care.
Removable Partial Denture
A removable partial denture is a dental appliance that can replace one or more missing teeth. It consists of artificial teeth attached to a gum-colored base, which is held in place using clasps or other attachments that grasp onto the remaining natural teeth. Removable partial dentures are a more affordable option compared to dental implants or bridges. They are removable for cleaning, but they may not provide the same stability and comfort as fixed options
Root Canal Aftercare Tips
After undergoing an endodontic procedure, it’s important to follow proper aftercare practices to ensure optimal healing and recovery. Here are some essential tips for root canal aftercare:
Take Prescribed Medications
Your dentist may prescribe antibiotics to prevent or treat any infection. Take the prescribed medications as directed, and finish the entire course. Pain medications or anti-inflammatory drugs may also be provided to manage any discomfort or swelling. Follow the instructions provided by your dentist or healthcare professional.
Avoid Chewing on the Treated Tooth
To allow the tooth to heal properly, avoid chewing on the treated tooth until the final restoration (dental crown or filling) is placed. Opt for soft foods and avoid sticky or hard foods that may cause damage or dislodgment of the temporary restoration.
Maintain Good Oral Hygiene
Continue to practice good oral hygiene by brushing your teeth twice a day and flossing daily. Use a soft-bristled toothbrush and a gentle touch around the treated tooth to avoid irritation. Rinse your mouth with an antimicrobial mouthwash to help control bacteria and maintain oral hygiene.
Rinse With Saltwater Solution
Rinse your mouth with a warm saltwater solution (one teaspoon of salt in a glass of warm water) a few times a day, especially after meals. This helps keep the area clean and reduces any swelling or discomfort.
Be Gentle During Brushing and Fossing
While maintaining oral hygiene, be gentle around the treated tooth to avoid putting excessive pressure on it. Use a toothbrush with soft bristles and a gentle, circular motion when brushing. When flossing, carefully maneuver the floss around the tooth, being cautious not to pull or dislodge any temporary or final restorations.
Avoid Extreme Temperatures and Pressure
During the healing period, avoid exposing the treated tooth to extreme temperatures, such as very hot or cold foods and beverages. Also, refrain from biting down on hard objects or using excessive force when chewing, as it may cause damage to the tooth or restorations.
Attend Follow-up Appointments
It is crucial to attend all scheduled follow-up appointments with your dentist. These appointments allow your dentist to monitor the healing process, remove any temporary restorations, and place the final restoration, such as a dental crown or filling. Follow your dentist’s recommendations regarding the timing and frequency of follow-up visits.
Report any Concerns or Issues
If you experience persistent pain, swelling, or any other unusual symptoms following the endodontic procedure, contact your dentist immediately. They will evaluate your situation and provide appropriate guidance or treatment if necessary.
FAQ
Here are some frequently asked questions (FAQs) on root canal treatment:
What is a Root Canal Treatment?
Root canal treatment, also referred to as endodontic treatment, is a dental procedure aimed at eliminating infected or damaged pulp within a tooth. The process entails thorough cleaning, disinfection, and subsequent filling of the tooth to prevent the recurrence of infection while restoring its original structure and functionality.
Why is a Root Canal Necessary?
A root canal is necessary when the pulp inside a tooth becomes infected or inflamed due to deep decay, repeated dental procedures, cracks or chips in the tooth, or trauma. If left untreated, the infection can spread, causing severe pain, abscess formation, and potential tooth loss.
Does Root Canal Treatment Hurt?
The endodontic procedure itself is performed under local anesthesia, so you should not feel any pain during the treatment. However, there may be some discomfort or sensitivity after the procedure, which can be managed with over-the-counter pain medications or as prescribed by your dentist.
How Long Does an Endodontic Procedure Take?
The duration of an endodontic procedure varies depending on the complexity of the case and the number of canals in the tooth. Generally, it can take one to three appointments, with each appointment lasting about 60 to 90 minutes.
What Happens After a Root Canal Treatment?
After a root canal, the tooth may be restored with a dental crown or filling to protect and strengthen it. You may experience some mild discomfort or sensitivity for a few days, which should gradually subside. It is important to maintain good oral hygiene and attend follow-up appointments as advised by your dentist.
Are There Any Alternatives to Root Canal Treatment?
In some cases, if a tooth is severely damaged or infected and cannot be saved through root canal treatment, extraction may be the only alternative. However, tooth extraction is typically followed by tooth replacement options such as dental implants, bridges, or removable dentures.
Can a Tooth That Had a Root Canal Treatment Get Re-Infected?
While root canal treatment has a high success rate, there is a slight possibility of re-infection if proper oral hygiene is not maintained or if there is a fracture or new decay in the tooth. Regular dental check-ups and practicing good oral hygiene are crucial to prevent re-infection and ensure the long-term success of the treated tooth.
How Long Does a Root Canal-Treated Tooth Last?
With proper care and maintenance, a root canal-treated tooth can last a lifetime. However, the longevity of the tooth depends on various factors, including oral hygiene practices, regular dental check-ups, and the overall health of the tooth and surrounding tissues.
Is Root Canal Treatment Expensive?
The cost of root canal treatment can vary due to several factors, including the specific tooth location, case complexity, and the fees charged by the dentist. Although root canal treatment may appear costly initially, it is often a more cost-effective solution in the long term when compared to tooth extraction followed by the need for tooth replacement options.
What is the Success Rate of an RCT?
The success rate of a root canal treatment is generally high, ranging from 85% to 95%. However, success depends on various factors such as the tooth’s condition, the expertise of the dentist, and the patient’s oral hygiene practices. Regular dental check-ups and proper maintenance are essential to ensure the long-term success of the treated tooth.
Which is Better Extraction or a Root Canal?
Determining whether extraction or a root canal is better depends on the specific situation and condition of the tooth. In general, preserving the natural tooth through a root canal is preferred whenever possible because it maintains the tooth’s function, and appearance, and helps preserve jawbone health. However, there are cases where extraction may be necessary if the tooth is severely damaged, infected beyond repair, or causing significant pain. Tooth extraction requires replacement options such as dental implants, bridges, or dentures to restore function and aesthetics. The decision should be made in consultation with a dental professional based on individual circumstances.
Is a Cap Necessary After RCT?
In most cases, a cap (dental crown) is necessary after a root canal treatment. A dental crown helps protect and strengthen the tooth, which may become brittle after the removal of infected pulp and the placement of a filling. Additionally, a dental crown restores the tooth’s natural appearance and provides long-term durability. However, there may be situations where a dental crown is not required, such as for front teeth with minimal damage or for temporary restorations. The need for a dental crown will be assessed by your dentist based on the specific condition of the treated tooth.
Do Teeth Weaken After a Root Canal?
Teeth can become more brittle and prone to fracture after a root canal treatment, especially if they are not properly restored with a dental crown. The removal of infected pulp and the subsequent filling of the root canal can cause the tooth to become slightly more fragile. However, placing a dental crown over the treated tooth provides added protection and strength, reducing the risk of fracture and restoring its functionality. Therefore, with a properly restored tooth, the weakening effect can be minimized, and the tooth can continue to function normally for many years.
Conclusion
In conclusion, root canal treatment, also known as endodontic treatment, is a highly effective dental procedure aimed at saving infected or damaged teeth. Throughout our conversation, we explored various aspects of root canal treatment, including its purpose, stages, steps, alternatives, aftercare, risks, and benefits.
Root canal treatment is recommended when the pulp inside a tooth becomes infected or inflamed due to factors like deep decay, trauma, or cracks. By removing the infected pulp, cleaning the root canals, and sealing them, the procedure alleviates pain, halts infection, and preserves the natural tooth. Dental crowns are often placed to restore strength and appearance.
While root canal treatment boasts high success rates, alternatives such as extraction followed by tooth replacement options like implants or bridges may be considered in certain cases. Proper aftercare, including medication adherence, good oral hygiene, and regular follow-up visits, is essential for successful healing and long-term maintenance.
Although temporary discomfort or sensitivity may occur, the benefits of root canal treatment outweigh the risks. Preserving the natural tooth allows for normal chewing, prevents adjacent teeth from shifting, and maintains a natural smile.
Ultimately, consult with a dental professional to assess your specific situation and make an informed decision about root canal treatment or alternative options tailored to your oral health needs.
Resources
Image Designed by freepik
References
https://www.ncbi.nlm.nih.gov/books/NBK470664/#:~:text=Root%20canal%2C%20or%20endodontic%20treatment,sealed%20with%20a%20restorative%20material.
https://www.ncbi.nlm.nih.gov/books/NBK587367/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9322405/
https://pubmed.ncbi.nlm.nih.gov/11307468/
https://www.sciencedaily.com/releases/2022/05/220517094850.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9322405/