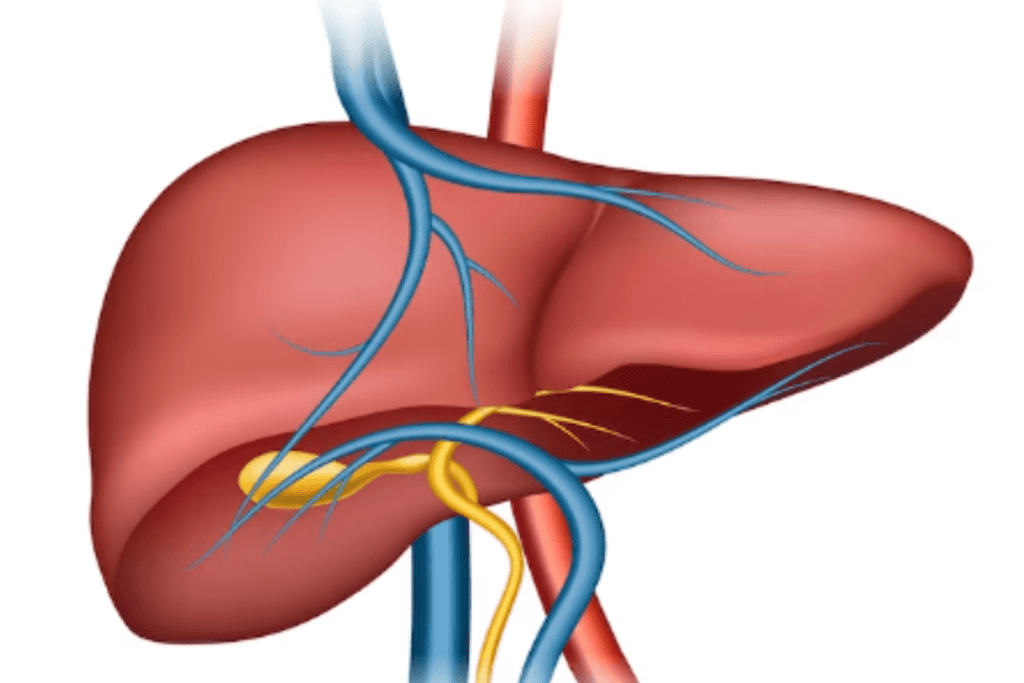
Liver fibrosis (Hepatic fibrosis) is a process in which the liver tissue becomes scarred and damaged due to prolonged inflammation and injury. As the liver tries to repair itself, excessive connective tissue, or scar tissue, forms, disrupting the normal structure and function of the liver. Over time, if not properly managed, severe hepatic fibrosis can progress to a more advanced condition known as cirrhosis, which can greatly impair liver function and lead to various complications.
Table of Contents
ToggleWhat are the Stages of Liver Fibrosis?
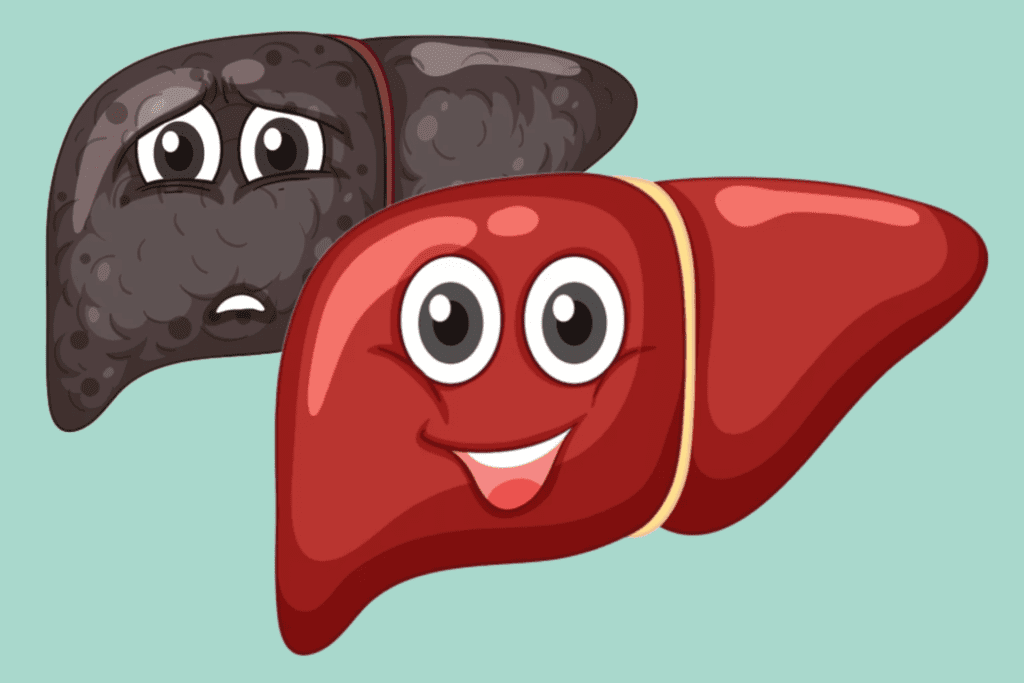
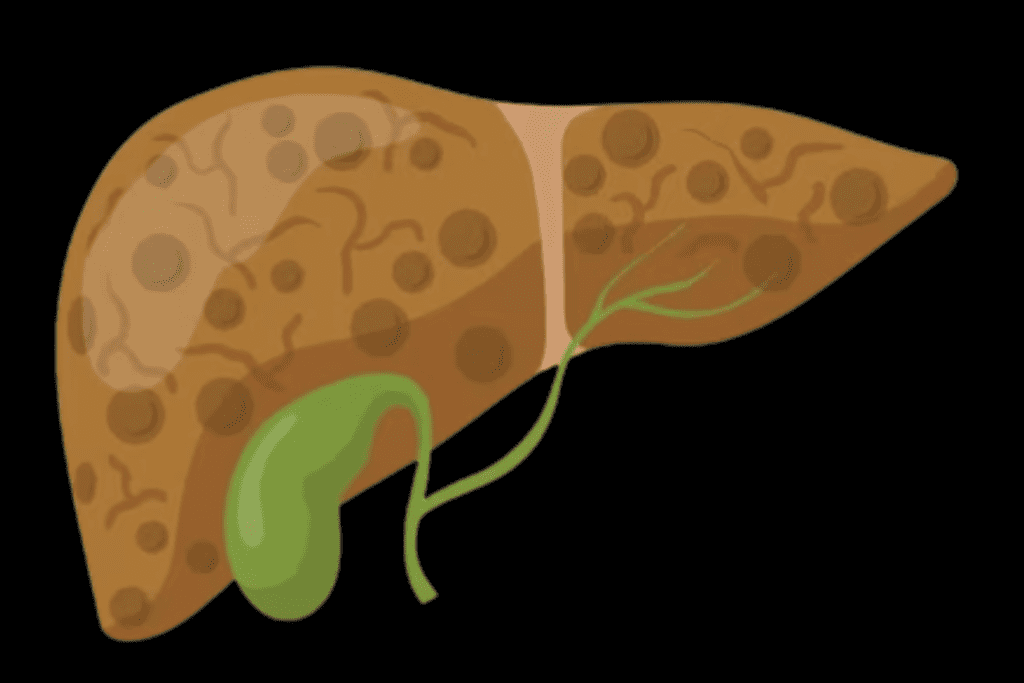
Liver fibrosis is commonly categorized into several stages, often using a numerical or alphabetical system, to indicate the extent of scar tissue accumulation and the progression of liver damage.
One commonly used staging system is the METAVIR scoring system, which uses a scale from F0 to F4:
F0: No Fibrosis
At this stage, there is no significant buildup of scar tissue in the liver. The liver tissue remains relatively healthy, and there is minimal to no disruption of its normal structure and function.
F1: Portal fibrosis
In this stage, there is mild fibrosis characterized by small amounts of scar tissue forming around the portal areas of the liver. Portal areas are regions where blood vessels, bile ducts, and other structures enter and exit the liver.
F2: Periportal Fibrosis
Fibrosis advances to a moderate level, with increased scarring around the portal areas. The scar tissue starts to expand and may extend slightly beyond the immediate portal regions.
F3: Bridging Fibrosis
At this point, the fibrosis becomes more significant. Bridging bands of scar tissue start to form, connecting one portal area to another. This can lead to the formation of larger scar structures that span across the liver.
F4: Cirrhosis
Cirrhosis is the ultimate phase of liver fibrosis progression. Scar tissue has extensively spread throughout the liver, leading to significant distortion of its architecture. Liver function is impaired, and complications such as portal hypertension (increased pressure in the liver’s blood vessels), ascites (fluid accumulation in the abdomen), and other health issues can arise.
What are the Symptoms of Hepatic fibrosis?
In the early stages of hepatic fibrosis, individuals often do not experience noticeable symptoms. As fibrosis progresses and the liver’s function becomes compromised, a range of symptoms may develop. However, it’s important to note that symptoms can vary widely and may be influenced by the underlying cause of fibrosis.
Some common symptoms and signs of advanced liver fibrosis or cirrhosis include:
Fatigue
Liver fibrosis can lead to reduced liver function, affecting the body’s ability to store and release energy. This can result in persistent fatigue and a feeling of low energy.
Jaundice
When the liver is unable to process bilirubin effectively, it can build up in the bloodstream and lead to yellowing of the skin and eyes, a condition known as jaundice.
Abdominal Swelling (Ascites)
Hepatic fibrosis can cause increased pressure in the blood vessels within the liver, leading to fluid leakage into the abdominal cavity. This can result in abdominal swelling and discomfort.
Easy Bruising and Bleeding
Liver dysfunction can affect the production of proteins necessary for blood clotting, leading to a higher likelihood of bruising and bleeding from minor injuries.
Itchy Skin
Accumulation of toxins in the bloodstream, along with reduced liver function, can lead to skin itching and irritation.
Loss of Appetite
Inflammation and damage to the liver can impact the body’s ability to process nutrients and metabolize food, leading to a decreased appetite and unintended weight loss.
Nausea and Vomiting
Liver fibrosis can disrupt the normal digestive process, leading to persistent nausea and vomiting.
Dark Urine
Excess bilirubin in the bloodstream can be excreted through the kidneys, leading to dark-colored urine.
Pale Stools
When bile production is compromised due to liver dysfunction, stools may appear pale or grayish.
Abdominal Pain
As fibrosis progresses and the liver becomes more inflamed, it can cause discomfort or pain in the upper right abdomen, where the liver is located.
Spider Angiomas
These are small, red, or purple blood vessels that appear on the skin, often resembling a spider’s web. They can be a visual sign of underlying liver dysfunction.
Enlarged Spleen
The spleen can enlarge as a result of increased pressure in the liver’s blood vessels, leading to further complications.
Confusion and Mental Changes (Hepatic Encephalopathy)
Advanced liver dysfunction can lead to a buildup of toxins in the bloodstream that can affect brain function, causing confusion, memory problems, and changes in behavior.
What are the Causes of Liver Fibrosis?
Liver fibrosis can be caused by a variety of factors that lead to chronic inflammation and damage to the liver cells.
Some common causes include:
Chronic Alcohol Consumption
Long-term and excessive alcohol consumption is a major contributor to hepatic fibrosis. Alcohol can directly damage liver cells and trigger inflammation, leading to scar tissue formation.
Viral Hepatitis
Chronic infections with hepatitis B or hepatitis C viruses can result in ongoing inflammation in the liver, which can lead to fibrosis over time.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD occurs when excess fat accumulates in the liver, often due to obesity and poor diet. In some cases, NAFLD can progress to non-alcoholic steatohepatitis (NASH), which involves inflammation and fibrosis.
Autoimmune Hepatitis
In autoimmune hepatitis, the immune system mistakenly attacks the liver cells, causing inflammation and potentially leading to fibrosis.
Chronic Exposure to Toxins and Medications
Long-term exposure to certain toxins, chemicals, or medications can damage liver cells and promote fibrosis. Examples include certain industrial chemicals, some prescription medications, and herbal supplements.
Genetic Disorders
Some genetic conditions, such as hemochromatosis (excessive iron accumulation) or Wilson’s disease (copper buildup), can cause liver inflammation and fibrosis.
Metabolic Disorders
Conditions like glycogen storage diseases and alpha-1 antitrypsin deficiency can impact liver function and contribute to fibrosis.
Autoimmune Diseases
Conditions like primary biliary cholangitis and primary sclerosing cholangitis involve inflammation and damage to the bile ducts, which can lead to fibrosis.
Cystic Fibrosis
This genetic disorder can affect various organs, including the liver, leading to fibrosis and other complications.
Cardiovascular Diseases
Certain heart conditions can lead to congestion in the liver’s blood vessels, causing inflammation and fibrosis.
How to Diagnose Liver Fibrosis
Diagnosing hepatic fibrosis involves a combination of medical assessments, tests, and imaging studies. A healthcare provider, often a hepatologist or gastroenterologist, will evaluate your medical history, symptoms, and risk factors before recommending specific diagnostic tests.
Here’s an overview of the common methods used to diagnose liver fibrosis:
Medical History and Physical Examination
Your doctor will ask about your medical history, including any known liver conditions, alcohol or drug use, and family history of liver diseases.
A physical examination may reveal signs such as jaundice, enlarged liver or spleen, or abdominal swelling.
Blood Tests
Liver function tests measure levels of liver enzymes and other markers in the blood to assess liver health and function. Tests for viral hepatitis (such as hepatitis B and C) can determine if infections are contributing to liver damage. Blood tests can also help evaluate blood clotting factors and the presence of inflammation.
Ultrasound
A non-invasive imaging technique that uses sound waves to create images of the liver and assess its size, shape, and blood flow.
FibroScan (Transient Elastography)
This test measures liver stiffness, which can indicate the degree of fibrosis. It’s a quick and painless procedure.
FibroTest or APRI (AST-to-Platelet Ratio Index)
These blood tests estimate the degree of fibrosis based on liver function and blood markers.
Biopsy
A liver biopsy entails extracting a small liver tissue sample for microscopic analysis, offering a direct evaluation of the extent and intensity of fibrosis.
While considered the gold standard, biopsies are invasive and carry some risks, so they are often reserved for cases where other methods are inconclusive.
Imaging Elastography
Techniques such as Magnetic Resonance Elastography (MRE) and Acoustic Radiation Force Impulse (ARFI) elastography use advanced imaging technology to assess liver stiffness and fibrosis without the need for a biopsy.
Specialized Blood Tests
Biomarker panels, like the Enhanced Liver Fibrosis (ELF) test, combine multiple blood markers to estimate fibrosis severity.
The choice of diagnostic method will depend on factors such as your medical history, the severity of your symptoms, and the availability of specific tests in your healthcare setting.
In some cases, a combination of tests may be used to accurately diagnose liver fibrosis and determine the appropriate treatment approach. It’s important to work closely with your healthcare provider to undergo the necessary tests and receive an accurate diagnosis.
Treatment Options for Hepatic fibrosis
The treatment of hepatic fibrosis aims to address the underlying causes, manage symptoms, and slow down or prevent further progression of fibrosis. The specific treatment approach will depend on the underlying condition causing the fibrosis, the stage of fibrosis, and individual patient factors. Here are some common treatment options:
Address Underlying Causes
For alcohol-related liver fibrosis, stopping or reducing alcohol consumption is crucial to prevent further damage.
Antiviral medications are used to treat chronic hepatitis B and C infections, which can help reduce inflammation and slow fibrosis progression.
Lifestyle changes, such as weight loss and improved diet, can be effective for managing non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH).
Medications
Some medications may help reduce inflammation and slow fibrosis progression. These can include corticosteroids, pentoxifylline, and certain targeted therapies depending on the underlying cause.
Antioxidant Supplements
Antioxidant supplements like vitamin E may be recommended in certain cases to help reduce oxidative stress and inflammation in the liver.
Manage Complications
Medications and procedures can help manage complications of advanced fibrosis, such as ascites (fluid accumulation), encephalopathy (brain dysfunction), and bleeding disorders.
Liver Transplantation
In severe cases of cirrhosis or advanced fibrosis, where the liver is significantly damaged and unable to function adequately, a liver transplant may be considered as a last option.
Clinical Trials
Experimental treatments and therapies may be available through clinical trials, particularly for conditions like NASH where there is ongoing research.
Healthy Lifestyle
Adopting a healthy lifestyle, including a balanced diet, regular exercise, weight management, and avoiding alcohol and harmful substances, can help improve liver health and slow fibrosis progression.
Regular Monitoring
Regular medical check-ups and monitoring are essential to track the progression of fibrosis and adjust treatment strategies as needed.
FAQ
Q1. What is hepatic fibrosis?
A1. Hepatic fibrosis is a process where scar tissue gradually forms in the liver due to chronic inflammation and injury. It is a response to ongoing damage and can lead to impaired liver function if left untreated.
Q2. What causes hepatic fibrosis?
A2. Hepatic fibrosis can be caused by factors like chronic alcohol consumption, viral hepatitis infections (B, C), non-alcoholic fatty liver disease (NAFLD), autoimmune disorders, and genetic conditions, among others.
Q3. What are the symptoms of hepatic fibrosis
A3. Symptoms include fatigue, jaundice (yellowing of skin/eyes), abdominal swelling (ascites), easy bruising, itching, loss of appetite, nausea, and more, as fibrosis progresses.
Q4. How is hepatic fibrosis diagnosed?
A4. Diagnosis involves a medical history, physical exams, blood tests, imaging (ultrasound, elastography), and sometimes liver biopsy for direct tissue assessment.
Q5. Can liver fibrosis be reversed?
A5. In its early stages, liver fibrosis can sometimes be reversible through lifestyle changes, treating underlying causes, and proper medical management.
Q6. What is the treatment for hepatic fibrosis?
A6. Treatment includes addressing underlying causes, medications to reduce inflammation, managing complications, adopting a healthy lifestyle, and, in severe cases, considering liver transplantation.
Q7. Is liver fibrosis the same as cirrhosis?
A7. No, cirrhosis is an advanced stage of liver fibrosis characterized by extensive scarring and significant disruption of liver function
Q8. How can liver fibrosis be prevented?
A8. Preventive measures include avoiding excessive alcohol consumption, getting vaccinated against hepatitis, maintaining a healthy weight, and managing conditions like diabetes and high cholesterol.
Q9. Can hepatic fibrosis lead to other complications?
A9. Yes, untreated hepatic fibrosis can progress to cirrhosis, which increases the risk of liver failure, liver cancer, and various complications affecting different body systems.
Q10. Why is early detection and management important?
A10. Early detection allows for timely intervention, which can slow down or even reverse fibrosis, preventing its progression to advanced stages and reducing the risk of serious complications.
Conclusion
Liver fibrosis is a progressive condition characterized by scar tissue formation in the liver due to various causes such as alcohol consumption, viral infections, and more. Its stages range from minimal scarring to advanced cirrhosis, impacting liver function and overall health. Early detection through blood tests, imaging, and biopsies is vital.
Treatment involves addressing underlying causes, lifestyle changes, medications, and in extreme cases, liver transplantation. Awareness of symptoms like fatigue, jaundice, and abdominal swelling is essential.
Collaborating with medical professionals helps manage hepatic fibrosis, enhancing the quality of life and preventing further damage. Regular monitoring, healthy habits, and adherence to treatments are key to maintaining liver health.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC546435
https://radiopaedia.org/articles/metavir-score-1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9479486/
https://www.msdmanuals.com/en-in/home/liver-and-gallbladder-disorders/fibrosis-and-cirrhosis-of-the-liver/fibrosis-of-the-liver
https://www.frontiersin.org/articles/10.3389/fphar.2022.874408/full