We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
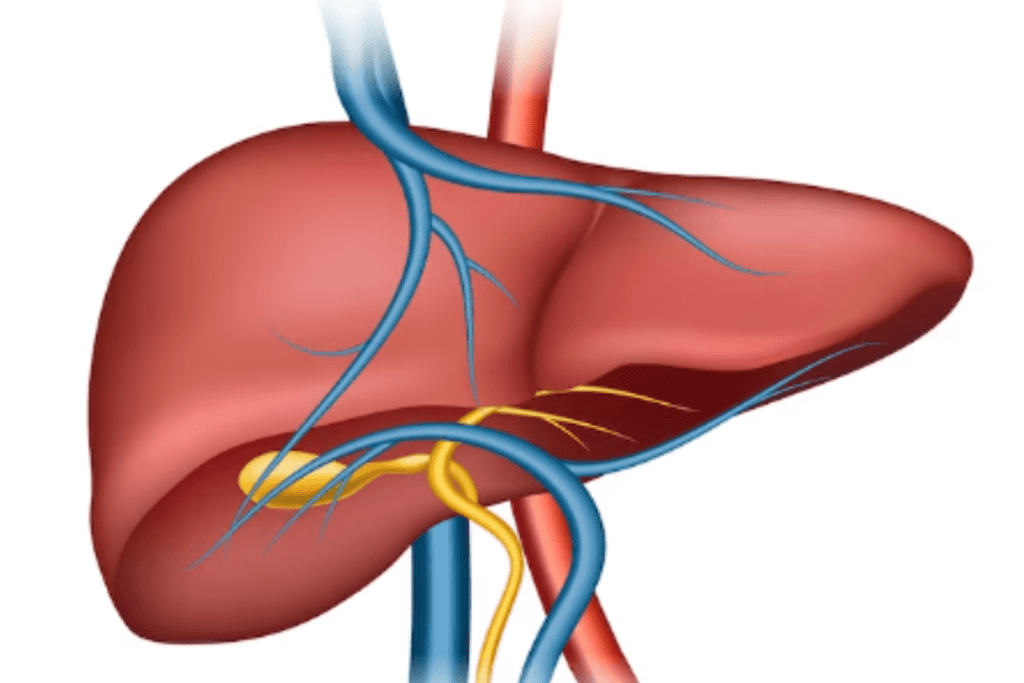
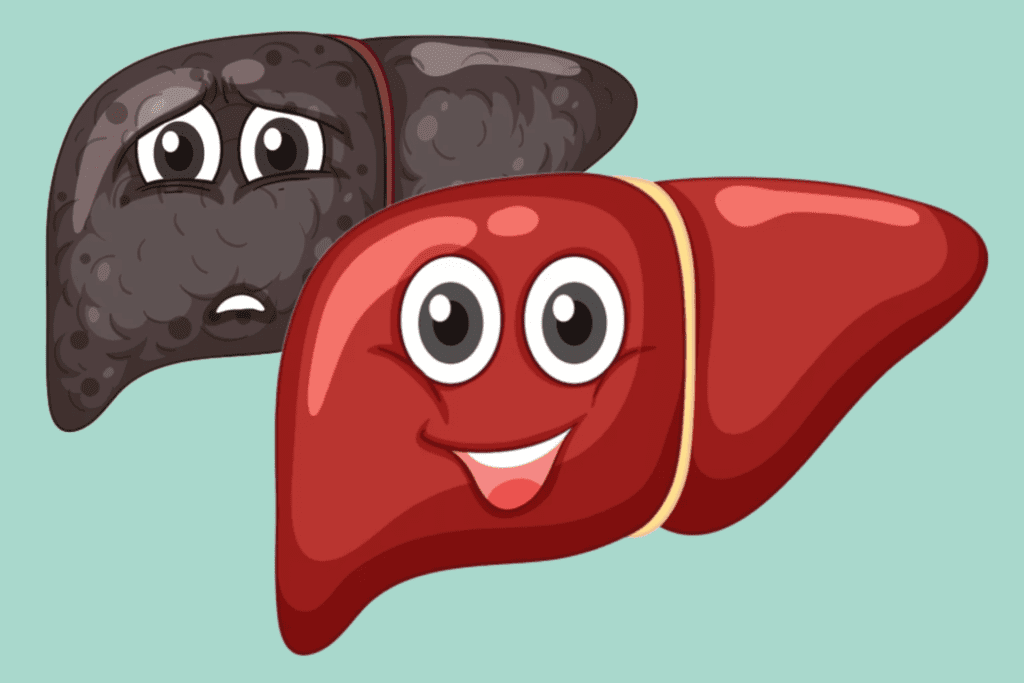
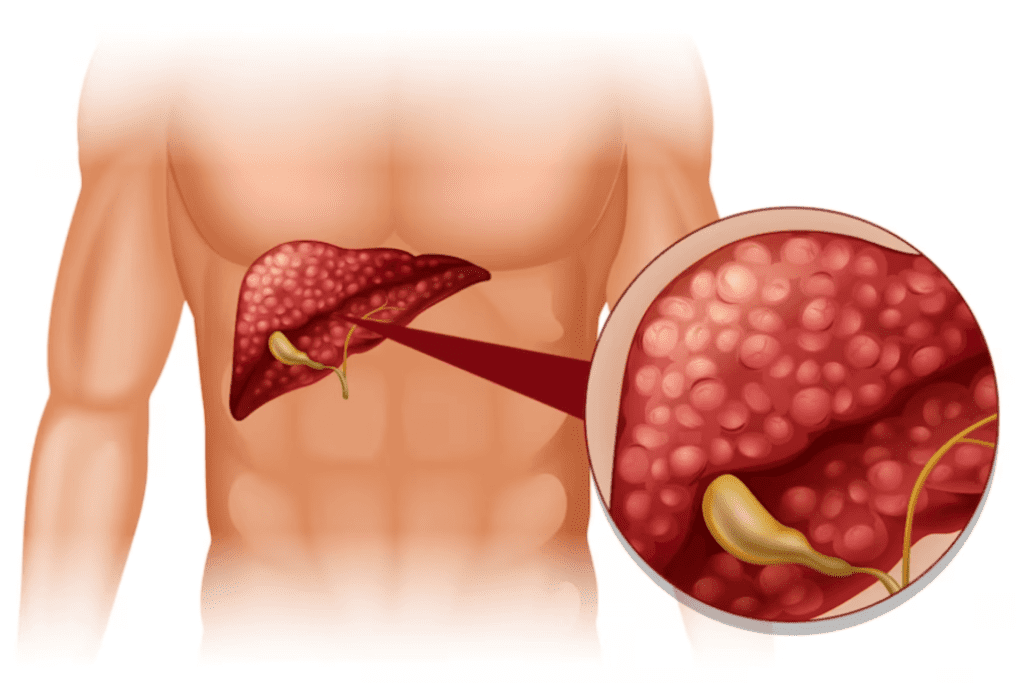
Liver cirrhosis is a severe and long-term liver condition marked by the gradual and permanent scarring (fibrosis) of liver tissue. This scarring replaces healthy liver cells, disrupting the liver’s regular structure and function. As the disease advances, the liver’s ability to perform its vital tasks, such as detoxification and metabolism, is compromised. Over time, cirrhosis can lead to liver dysfunction and the emergence of serious complications.
Table of Contents
ToggleIn this article, we delve into the stages, types, causes, symptoms, diagnosis, treatment, and prevention of cirrhosis, aiming to shed light on this critical health concern.
Stages
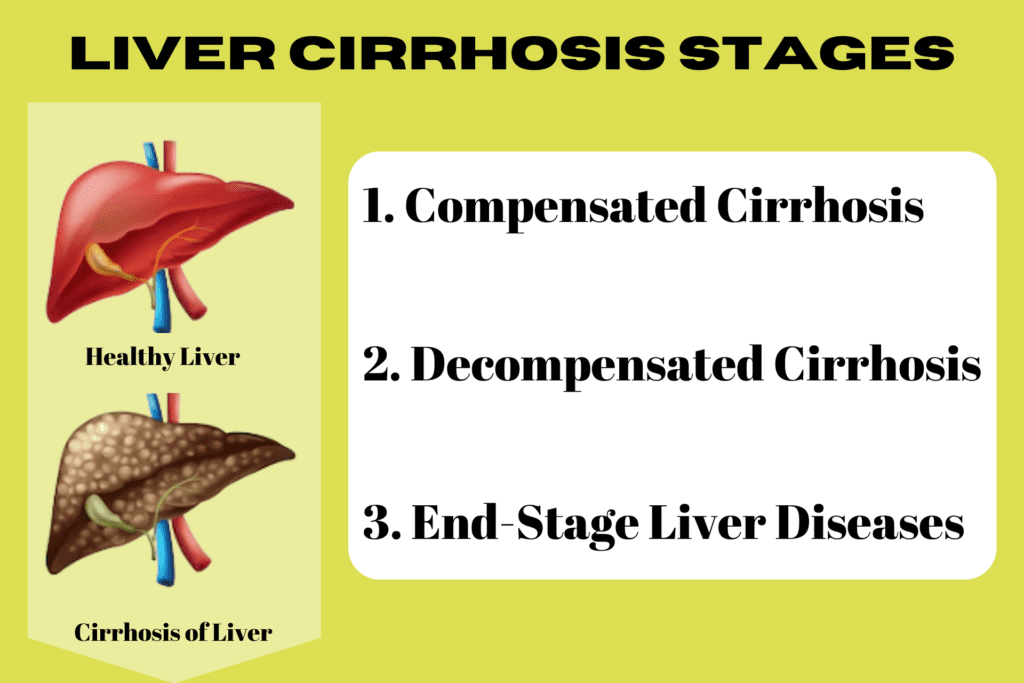
Liver cirrhosis typically progresses through several stages, each characterized by the severity of liver damage and the extent of scarring. The Child-Pugh classification and the Model for End-Stage Liver Disease (MELD) score are widely employed as the primary staging systems for cirrhosis.
Here are the general stages of liver cirrhosis:
1. Compensated Cirrhosis (Early Stage)
In this stage, the liver damage is mild to moderate, and the liver can still perform most of its functions adequately. Symptoms may be minimal or absent. With appropriate medical management and lifestyle changes, the liver can compensate for the damage.
2. Decompensated Cirrhosis (Advanced Stage)
As cirrhosis progresses, the liver’s ability to function declines significantly, and complications start to emerge. Symptoms become more apparent, including fatigue, jaundice, swelling, and easy bruising. Complications like ascites (fluid accumulation in the abdomen), hepatic encephalopathy (brain dysfunction), and variceal bleeding (bleeding from enlarged veins in the esophagus or stomach) may occur.
3. End-Stage Liver Disease
In this final stage, the liver function is severely impaired, and complications are life-threatening. Liver failure may occur, leading to a critical condition that requires urgent medical intervention. Liver transplantation becomes a consideration for some patients at this stage.
Types and Causes
Liver cirrhosis is generally classified based on its underlying causes or etiology.
The common types of liver cirrhosis include:
Alcoholic Cirrhosis
Alcoholic cirrhosis is the most common type of cirrhosis and is caused by long-term, excessive alcohol consumption. Alcohol is toxic to liver cells, and chronic alcohol abuse can lead to inflammation and damage, causing scar tissue to form. As the condition progresses, the liver’s ability to function declines, and cirrhosis develops.
Non-Alcoholic Fatty Liver Disease (NAFLD) / Non-Alcoholic Steatohepatitis (NASH)
NAFLD occurs when fat accumulates in the liver cells due to factors unrelated to alcohol consumption. Over time, some people with NAFLD may develop NASH, where inflammation and liver cell damage occur alongside fat accumulation. NASH can progress to fibrosis, and cirrhosis, ultimately resulting in liver failure.
Chronic Viral Hepatitis Cirrhosis
Chronic viral hepatitis, particularly hepatitis B (HBV) or hepatitis C (HCV), can lead to liver cirrhosis if left untreated. These viruses cause ongoing inflammation in the liver, leading to liver cell damage and fibrosis over time.
Autoimmune Hepatitis Cirrhosis
In autoimmune hepatitis, the body’s immune system mistakenly attacks the liver cells, leading to inflammation and damage. If left untreated or inadequately managed, this ongoing immune response can lead to cirrhosis.
Primary Biliary Cirrhosis (PBC)
PBC is an autoimmune disease that primarily affects the small bile ducts within the liver. The immune system attacks these bile ducts, leading to their inflammation and destruction. As the disease progresses, bile duct damage can cause liver cell injury and cirrhosis.
Primary Sclerosing Cholangitis (PSC)
Similar to PBC, PSC is an autoimmune disorder, but it primarily affects the larger bile ducts in and around the liver. In PSC, the bile ducts become inflamed, scarred, and narrowed, which can obstruct the flow of bile and lead to liver damage and cirrhosis.
Hemochromatosis
Hemochromatosis is a genetic disorder where the body absorbs and stores excessive amounts of iron from the diet. This leads to iron overload in various organs, including the liver, causing liver cell damage and cirrhosis.
Wilson's Disease
Wilson’s disease is a rare inherited disorder that impairs the body’s ability to eliminate excess copper, resulting in copper buildup in various organs, including the liver. Over time, the accumulated copper damages liver cells and can lead to cirrhosis.
Medications and Toxins
Certain medications and exposure to toxins or chemicals can cause liver damage and, in some cases, progress to cirrhosis.
Cystic Fibrosis
People with cystic fibrosis have a higher risk of developing cirrhosis due to the buildup of thick mucus in the liver.
Other Rare Causes
There are several other rare causes of cirrhosis, including certain genetic and metabolic disorders.
Symptoms
The symptoms of cirrhosis can vary depending on the stage of the disease and the extent of liver damage. In the early stages of compensated cirrhosis, symptoms may be mild or even absent. However, as cirrhosis progresses and the liver function declines, the following symptoms may become more noticeable:
Fatigue and Weakness
The liver plays a crucial role in energy metabolism and storage. As cirrhosis progresses, the liver’s ability to store and release energy in the form of glucose and glycogen is impaired. This leads to persistent fatigue and weakness, making it challenging for individuals with cirrhosis to carry out daily activities.
Jaundice
Jaundice occurs when the liver is unable to properly process and eliminate bilirubin, a waste product produced from the breakdown of old red blood cells. The buildup of bilirubin in the bloodstream results in a yellowish discoloration of the skin and the whites of the eyes.
Itchy Skin (Pruritus)
Elevated levels of bile salts in the bloodstream can cause itching or pruritus. Bile salts are normally released by the liver to aid in digestion, but when the liver is damaged, these compounds may accumulate in the skin and cause irritation.
Abdominal Pain and Swelling
As cirrhosis progresses, it can lead to portal hypertension, an increase in blood pressure within the portal vein that carries blood from the digestive organs to the liver. Portal hypertension can cause abdominal pain and discomfort. Additionally, liver damage can lead to the accumulation of fluid in the abdominal cavity, resulting in abdominal swelling or ascites.
Easy Bruising and Bleeding
The liver plays a key role in producing clotting factors that help prevent excessive bleeding. In cirrhosis, the liver’s ability to synthesize these clotting factors is impaired, leading to easy bruising and prolonged bleeding from minor injuries.
Spider-Like Blood Vessels (Spider Angiomas)
Cirrhosis can cause changes in blood flow and increased pressure in certain blood vessels. This can result in the appearance of small, reddish skin lesions known as spider angiomas or spider nevi.
Swelling in the Legs and Ankles
Edema, or swelling, in the legs and ankles, can occur due to fluid retention caused by impaired liver function and changes in blood flow.
Weight Loss and Loss of Appetite
As cirrhosis progresses, individuals may experience a reduced appetite and unintended weight loss. This can be attributed to a combination of factors, including nausea, malabsorption of nutrients, and metabolic changes.
Nausea and Vomiting
Digestive disturbances are common in cirrhosis patients, and these can lead to symptoms like nausea and vomiting.
Mental Confusion and Personality Changes (Hepatic Encephalopathy)
Hepatic encephalopathy is a condition that occurs when the liver is unable to remove toxins, particularly ammonia, from the blood. The accumulation of toxins in the brain can lead to cognitive impairment, confusion, memory loss, and changes in behavior and personality.
Gynecomastia in Men
Cirrhosis can disrupt hormonal balance, leading to an increase in estrogen levels in men. This hormonal imbalance can cause gynecomastia, which is the enlargement of breast tissue in males.
Diagnosis
Diagnosing liver cirrhosis involves a combination of medical history, physical examination, laboratory tests, imaging studies, and sometimes, a liver biopsy.
Here are the steps typically involved in the diagnostic process:
Medical History and Physical Examination
Your healthcare provider will ask about your medical history, including any symptoms you may be experiencing. They will also inquire about risk factors for liver disease, such as alcohol consumption, hepatitis infections, and exposure to certain toxins.
Blood Tests
Blood tests are essential for evaluating liver function and identifying markers of liver damage. Common blood tests include liver function tests (LFTs), which measure liver enzyme levels, bilirubin, and albumin. Other tests may include viral hepatitis serology to check for hepatitis A, B, and C, as well as other specific markers related to liver health.
Imaging Studies
Imaging tests can provide valuable information about the liver’s size, shape, and structure. Common imaging modalities used to diagnose cirrhosis include:
Ultrasound:
This non-invasive imaging technique uses sound waves to create pictures of the liver. Ultrasound can show liver enlargement, ascites, and signs of cirrhosis.
Computed Tomography (CT) Scan:
A CT scan provides detailed cross-sectional images of the liver, helping to visualize liver nodules, fibrosis, or signs of advanced cirrhosis.
Magnetic Resonance Imaging (MRI):
Like CT, MRI can provide detailed images of the liver and surrounding structures, helping to evaluate liver health and detect cirrhosis.
FibroScan or Transient Elastography:
These are specialized ultrasound-based tests that assess liver stiffness, a parameter related to fibrosis severity.
Liver Biopsy
Occasionally, a liver biopsy may be required to verify the diagnosis and evaluate the level of liver damage. In this procedure, a tiny sample of liver tissue is extracted and examined under a microscope to detect the presence and severity of fibrosis and cirrhosis.
Other Tests
Additional tests may be ordered to evaluate liver function and assess for complications related to cirrhosis, such as assessing for portal hypertension, esophageal varices, and kidney function.
Treatment
The treatment of liver cirrhosis depends on the underlying cause and the stage of the disease. The primary goals of treatment are to manage the symptoms, slow down the progression of cirrhosis, prevent complications, and improve the overall quality of life.
Here are some common approaches to the treatment of liver cirrhosis:
Lifestyle Changes
For individuals with alcoholic cirrhosis or non-alcoholic fatty liver disease (NAFLD)/non-alcoholic steatohepatitis (NASH), the first step is often to make lifestyle changes. This includes abstaining from alcohol consumption for alcoholic cirrhosis and adopting a healthy diet and regular exercise for NAFLD/NASH.
Medications
Medications may be prescribed to manage specific complications and symptoms associated with cirrhosis. For example, diuretics may be used to reduce fluid retention and swelling (ascites). Lactulose or other medications can be prescribed to treat hepatic encephalopathy.
Treating Underlying Conditions
If cirrhosis is caused by chronic viral hepatitis, antiviral medications may be used to control the viral infection and reduce liver inflammation. Autoimmune liver diseases may require immunosuppressive medications to dampen the immune response.
Managing Complications
Depending on the severity of cirrhosis, various complications may arise. These can include variceal bleeding, infections, kidney problems, and more. Prompt medical intervention and treatment are essential to manage these complications effectively.
Managing Complications
Depending on the severity of cirrhosis, various complications may arise. These can include variceal bleeding, infections, kidney problems, and more. Prompt medical intervention and treatment are essential to manage these complications effectively.
Liver Transplantation
For individuals with advanced cirrhosis and liver failure, a liver transplant may be considered. A liver transplant involves replacing the damaged liver with a healthy liver from a deceased or living donor. This is often the last resort when other treatments are not sufficient.
Regular Monitoring
People with cirrhosis require regular check-ups and monitoring to assess liver function, detect complications early, and adjust the treatment plan as needed.
Avoiding Certain Medications and Toxins
People with cirrhosis should avoid medications and substances that can further damage the liver, such as certain painkillers, herbal supplements, and alcohol.
Prevention
Preventing liver cirrhosis involves adopting a healthy lifestyle and making choices that protect the liver from damage.
Here are some key steps to help prevent liver cirrhosis:
Limit Alcohol Consumption
To minimize the risk of cirrhosis, consume alcohol in moderation. For women, this generally means limiting intake to one drink per day, while men can have up to two drinks per day. Avoid excessive or binge drinking, as chronic alcohol abuse is a primary factor contributing to cirrhosis.
Maintain a Healthy Diet
Maintain a well-balanced diet comprising a diverse range of fruits, vegetables, whole grains, and lean proteins. Minimize intake of processed foods, sugary beverages, and unhealthy fats. If you have obesity or diabetes, collaborate with a healthcare professional to effectively manage these conditions. A healthy diet is essential for reducing the risk of liver-related complications, including cirrhosis.
Prevent Viral Hepatitis
Get vaccinated against hepatitis A and B, and avoid behaviors that can lead to hepatitis transmission, such as unprotected sex and sharing needles.
Practice Safe Sex
Use condoms consistently to reduce the risk of sexually transmitted infections that can lead to hepatitis.
Avoid Injecting Drugs
If you use illicit drugs, avoid sharing needles and seek help to quit or reduce drug use.
Exercise Regularly
Engage in regular physical activity as it can help improve liver health and reduce the risk of obesity and other related conditions.
Avoid Toxins
Be cautious with household chemicals, medications, and substances that can harm the liver. Follow instructions for medications and avoid self-medicating or combining medications without consulting a healthcare provider.
Practice Safe Tattooing and Piercing
Ensure that tattoo and piercing parlors follow proper hygiene and safety practices to prevent infection with hepatitis or other blood-borne viruses.
Get Regular Medical Check-ups
Make it a habit to regularly attend check-ups and screenings with your healthcare provider. Early detection and treatment of liver diseases can help prevent cirrhosis or slow its progression.
Be Cautious with Herbal Supplements
Be aware that some herbal supplements may interact with medications or have adverse effects on the liver. Before using any herbal products, seek advice from a healthcare provider.
Limit Exposure to Environmental Toxins
Be cautious about exposure to chemicals and toxins in the workplace or the environment that can affect liver health.
Conclusion
In conclusion, liver cirrhosis is a serious and progressive condition characterized by the irreversible scarring of liver tissue, leading to impaired liver function and potential complications. The disease can be caused by various factors, including chronic alcohol abuse, viral hepatitis, fatty liver disease, and autoimmune disorders. Early detection and appropriate management are essential for slowing the disease’s progression and preventing severe complications. Lifestyle changes, such as limiting alcohol consumption, adopting a healthy diet, and exercising regularly, can play a significant role in preventing liver cirrhosis. Additionally, vaccination against hepatitis, safe sex practices, and avoidance of harmful substances can reduce the risk of developing cirrhosis. Regular medical check-ups and timely interventions are crucial in ensuring better outcomes for individuals with liver cirrhosis.
References
https://www.hepatitis.va.gov/
https://www.ncbi.nlm.nih.gov/books/NBK482419/
https://www.nhs.uk/conditions/cirrhosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3583179/
https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis/treatment