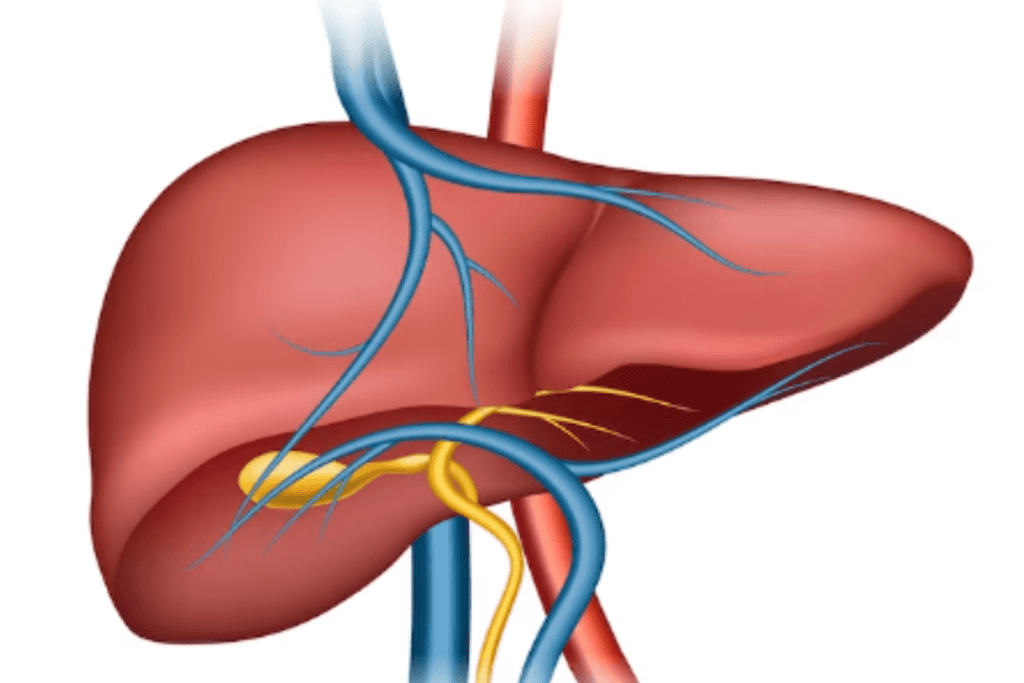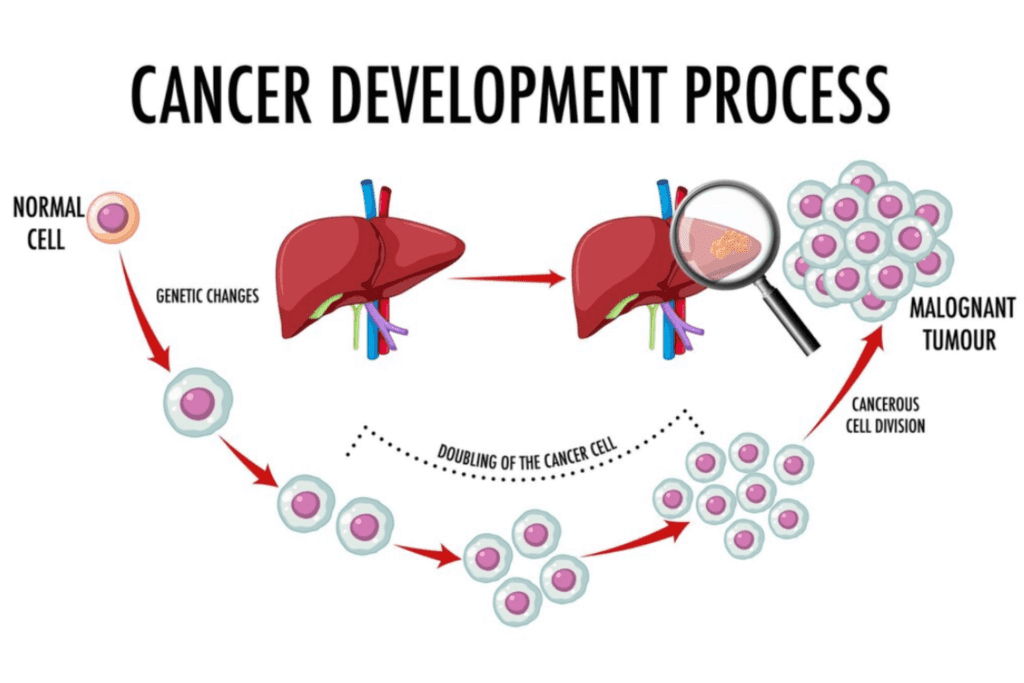
Hepatocellular carcinoma (HCC) is a primary liver cancer that originates from hepatocytes, the main cells of the liver. It’s one of the most common types of liver cancer and is often associated with underlying liver diseases, such as cirrhosis caused by chronic viral hepatitis or alcohol abuse. HCC tends to exhibit aggressive growth and may have limited symptoms in its early stages, making early detection challenging. It poses a significant global health concern due to its potential for rapid progression and limited treatment options in advanced stages. Regular surveillance and timely interventions are crucial for managing HCC effectively.
Table of Contents
ToggleHow Many Stages of Hepatocellular Carcinoma are There?
Hepatocellular carcinoma (HCC) is commonly staged using the Barcelona Clinic Liver Cancer (BCLC) system, which categorizes the disease into several stages based on factors such as tumor size, liver function, and overall health of the patient.
The BCLC system includes the following stages:
Very Early Stage
At this stage, HCC is characterized by a single small tumor that is less than 2 cm in size. The tumor has not spread to nearby blood vessels or lymph nodes. The liver function is well-preserved, as indicated by a Child-Pugh score of A. This stage is often considered the most favorable for treatment, and options may include surgical resection, local ablation therapies, or transplantation.
Early Stage
In the early stage, HCC is still confined to the liver. There are two subcategories within this stage:
- A single tumor that is larger than 2 cm but less than 5 cm in size
- Multiple small tumors, each less than 3 cm in size.
Liver function remains relatively preserved (Child-Pugh A). Treatment options include surgical resection, liver transplantation, and local therapies such as radiofrequency ablation or transarterial chemoembolization (TACE).
Intermediate Stage
At this stage, HCC may involve larger tumors or multiple tumors in the liver. Some tumors might have extended into nearby blood vessels but have not yet spread to distant parts of the body. Liver function can vary, and patients might fall into Child-Pugh class A or B. Treatment options might involve TACE, radioembolization, or targeted therapies, depending on the individual’s health status and tumor characteristics.
Advanced Stage
HCC has reached an advanced stage when it has either spread to other parts of the body (metastasis) or significantly compromised liver function. This stage includes multiple tumor nodules, vascular invasion, or lymph node involvement. Treatment options might include systemic therapies like sorafenib, lenvatinib, or immunotherapy. In some cases, local therapies might still be considered to manage symptoms.
End-Stage
The end-stage of HCC is characterized by extensive tumor involvement and severe liver dysfunction. At this point, treatment options become limited, and the focus shifts towards supportive care to manage symptoms and improve the patient’s quality of life. Palliative care measures, such as pain management and addressing complications, are central.
Hepatocellular Carcinoma Causes
Hepatocellular carcinoma (HCC) is a complex disease with multiple risk factors that can contribute to its development.
Some of the main causes and risk factors for HCC include:
Chronic Viral Hepatitis Infections
Chronic infections with hepatitis B virus (HBV) or hepatitis C virus (HCV) are significant contributors to HCC. These viruses attack the liver, leading to ongoing inflammation and potential scarring (cirrhosis). Continuous inflammation can cause DNA damage and mutations in liver cells, eventually leading to cancer.
Cirrhosis
Cirrhosis is a late-stage liver condition where healthy liver tissue is replaced by scar tissue. It can result from various causes, including viral hepatitis, alcohol abuse, NAFLD/NASH, and autoimmune diseases. Cirrhosis provides an environment for genetic mutations that can promote the growth of cancer cells.
Alcohol Abuse
Excessive and prolonged alcohol consumption damages liver cells, leading to inflammation and cirrhosis. Chronic liver inflammation promotes cell division and genetic changes, increasing the risk of HCC over time.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD involves fat accumulation in the liver cells due to factors like obesity and insulin resistance. If left unchecked, NAFLD can progress to NASH, where inflammation and damage occur. NASH-related cirrhosis raises the risk of HCC.
Aflatoxin Exposure
Aflatoxins, produced by molds found in certain foods, are potent carcinogens. Chronic exposure, mainly in areas with poor food storage practices, can lead to DNA damage in liver cells, increasing the risk of HCC.
Metabolic Syndrome
Conditions like obesity, type 2 diabetes, and high blood pressure contribute to metabolic syndrome. These factors increase liver inflammation and fat accumulation, promoting liver damage and possibly HCC development.
Genetic Factors
Genetic conditions like hereditary hemochromatosis (excess iron absorption) and alpha-1 antitrypsin deficiency (an enzyme disorder) affect the liver’s function and can lead to liver diseases that raise HCC risk.
Cigarette Smoking
Smoking introduces harmful substances into the body, creating oxidative stress and inflammation. These factors can contribute to liver cell damage and an increased risk of HCC.
Certain Medications
Prolonged use of anabolic steroids and certain antiviral drugs can cause liver damage and inflammation, potentially increasing the likelihood of HCC.
Environmental Toxins
Exposure to environmental toxins like vinyl chloride (used in plastics manufacturing) and arsenic can lead to liver damage and inflammation, creating an environment conducive to HCC development.
Gender and Age
Men tend to have a higher risk of HCC than women. Additionally, as people age, accumulated exposure to risk factors and natural changes in the liver’s regenerative capacity increase the risk of HCC.
What are the Hepatocellular Carcinoma Symptoms
Hepatocellular carcinoma (HCC) symptoms can vary depending on the stage of the disease and its impact on the liver. In the early stages, HCC might not cause noticeable symptoms, while in later stages, as the tumor grows and affects liver function, symptoms become more apparent.
Common symptoms of hepatocellular carcinoma include:
Abdominal Pain
Pain or discomfort in the upper right side of the abdomen, where the liver is located, can occur as the tumor grows and exerts pressure on surrounding tissues.
Unintended Weight Loss
Significant weight loss without any change in diet or physical activity can be a sign of advanced HCC. This weight loss is often due to the body’s increased energy expenditure caused by the cancer.
Loss of Appetite
Decreased appetite and aversion to food are common, possibly due to the cancer’s impact on metabolism and liver function.
Jaundice
Jaundice is identified by the yellow discoloration of the skin and eyes. It occurs when the liver cannot effectively process bilirubin, leading to its buildup in the body. HCC can obstruct bile ducts, causing jaundice.
Fatigue
HCC and its impact on liver function can lead to fatigue and weakness, even with normal activity levels.
Abdominal Swelling
Enlargement of the liver or the accumulation of fluid in the abdomen (ascites) can lead to abdominal swelling and discomfort.
Easy Bruising and Bleeding
A damaged liver may not produce enough clotting factors, leading to easy bruising and bleeding.
Nausea and Vomiting
Liver dysfunction and the accumulation of waste products in the blood can lead to nausea and vomiting.
Changes in Bowel Movements
Changes in bowel habits, such as dark or tar-like stools (indicating upper gastrointestinal bleeding) or pale stools (indicating issues with bile flow), can be observed.
Enlarged Liver
An enlarged liver can often be felt by a doctor during a physical examination.
Spider Angiomas
These are small, red, spider-like blood vessels that may appear on the skin due to altered blood flow resulting from liver dysfunction.
Fever
Some individuals with HCC may experience fever as a result of infection or inflammation related to the cancer.
How to HCC Diagnose
The diagnosis of hepatocellular carcinoma (HCC) involves a combination of medical history, physical examination, imaging studies, and sometimes laboratory tests. Timely and accurate diagnosis is crucial for determining the appropriate treatment strategy.
Here’s an overview of the diagnostic process for HCC:
Medical History and Physical Examination
A healthcare provider will take a detailed medical history, including risk factors like hepatitis, cirrhosis, alcohol consumption, and family history of liver diseases. A physical examination may also reveal signs such as an enlarged liver, jaundice, or abdominal swelling.
Imaging Studies
Various imaging techniques are used to visualize the liver and detect any abnormalities.
Common imaging methods include:
Ultrasound:
A non-invasive technique that uses sound waves to create images of the liver.
Computed Tomography (CT) Scan:
A detailed X-ray imaging technique that provides cross-sectional images of the liver.
Magnetic Resonance Imaging (MRI):
Utilizes powerful magnetic fields and radio waves to generate intricate images of the liver.
Angiography:
A procedure that involves injecting a contrast dye into blood vessels to visualize blood flow within the liver.
Blood Tests
Blood tests can help assess liver function, identify hepatitis infections, and detect tumor markers. Alpha-fetoprotein (AFP) is a common tumor marker associated with HCC, although elevated AFP levels can also be present in other conditions.
Biopsy
In some cases, a biopsy may be performed to confirm the presence of HCC. A small sample of liver tissue is taken for analysis to determine if cancer cells are present. However, biopsies are not always necessary if imaging studies and clinical history strongly suggest HCC, as the biopsy procedure carries some risks.
Staging and Further Evaluation
If HCC is confirmed, further evaluation is done to determine the stage of the cancer, which helps guide treatment decisions. Staging includes assessing the size and number of tumors, involvement of blood vessels, and whether the cancer has spread to other parts of the body.
Multidisciplinary Discussion
Based on the diagnosis and staging, a team of medical professionals including oncologists, hepatologists, radiologists, and surgeons may meet to discuss the best treatment options for the individual.
Hepatocellular Carcinoma Treatment
The treatment of hepatocellular carcinoma (HCC) depends on several factors, including the stage of cancer, the patient’s overall health, the presence of underlying liver disease, and the available treatment options. HCC management often involves a multidisciplinary approach, including oncologists, hepatologists, surgeons, radiologists, and other specialists.
Here are some common treatment options for HCC:
1. Surgery
Surgical Resection:
This involves surgically removing the tumor along with a portion of the healthy liver tissue around it. It’s considered for early-stage HCC and requires sufficient liver function to tolerate the removal of tissue.
Liver Transplantation:
In selected cases, a liver transplant may be an option for patients with small tumors and well-compensated cirrhosis. The entire liver is replaced with a healthy donor liver, effectively removing both the tumor and the underlying liver disease.
2. Ablation Therapies
Radiofrequency Ablation (RFA):
A thin needle is inserted into the tumor, and radiofrequency energy is used to heat and destroy cancer cells. It’s effective for small tumors and can be performed using minimally invasive techniques.
Microwave Ablation:
Similar to RFA, but using microwaves to heat and destroy cancer cells. It might be used when RFA is not feasible.
Ethanol Ablation (PEI):
Pure ethanol is injected directly into the tumor, causing the cancer cells to die due to cell dehydration.
3. Transarterial Therapies
Transarterial Chemoembolization (TACE):
A catheter is inserted into the blood vessels supplying the tumor. Chemotherapy drugs are infused directly into the tumor, followed by embolization to block blood flow and trap the drugs within the tumor.
Transarterial Radioembolization (TARE):
Tiny radioactive beads are delivered to the tumor’s blood vessels, emitting radiation that damages the cancer cells.
4. Systemic Therapies
Targeted Therapies:
These drugs inhibit specific molecules involved in cancer growth. Sorafenib, lenvatinib, and regorafenib are examples used in advanced HCC.
Immunotherapy:
Immune checkpoint inhibitors like nivolumab and pembrolizumab are being explored for HCC treatment. These drugs help the immune system target and attack cancer cells.
Chemotherapy:
Traditional chemotherapy drugs are less commonly used in HCC due to limited effectiveness compared to other treatments.
5. Supportive Care
Palliative care focuses on alleviating symptoms and improving the patient’s quality of life. It addresses pain management, emotional support, and symptom relief for advanced-stage HCC patients.
6. Clinical Trials
Clinical trials involve testing new treatments or combinations of existing treatments to improve HCC outcomes. Participation in trials can provide access to cutting-edge therapies that may offer benefits beyond standard options.
Hepatocellular Carcinoma icd-10 Code
ICD-10 stands for the “International Classification of Diseases, 10th Revision.” It’s a standardized system used worldwide to classify and code various diseases, medical conditions, and health-related issues for billing, statistical analysis, and tracking health trends. Each disease or condition is assigned a specific alphanumeric code.
The ICD-10 code for hepatocellular carcinoma (HCC) is “C22.0.”
Now, let’s analyze the elements of this code:
C: The first character of the code, in this case, “C,” represents the chapter of the ICD-10 system. The chapter “C” is dedicated to diseases of the digestive system, including various gastrointestinal malignancies.
22: The second and third characters further narrow down the classification. In the ICD-10 system, “C22” specifically refers to malignant neoplasms (cancers) of the liver and intrahepatic bile ducts.
.0: The last character is an extension that adds specificity to the code. In this case, “.0” signifies that the code pertains to the primary malignant neoplasm of the liver.
So, when you see the ICD-10 code “C22.0,” it indicates that the patient has been diagnosed with a primary malignant neoplasm (cancer) located in the liver. This code is used by healthcare professionals for medical documentation, insurance claims, and statistical reporting. It helps ensure accurate communication about the specific disease or condition being diagnosed and treated.
Conclusion
In conclusion, hepatocellular carcinoma’s multifaceted nature demands a holistic approach. A clear understanding of its causes, vigilant symptom monitoring, accurate diagnosis, and personalized treatment strategies are vital in addressing this challenging cancer. The ever-advancing field of oncology offers hope, emphasizing the importance of staying informed and working closely with healthcare experts for the best possible outcomes.
Resources
Image Designed by Freepik
References
https://www.ncbi.nlm.nih.gov/books/NBK559177/
https://www.ncbi.nlm.nih.gov/books/NBK448337/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4014047/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3989948/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023919/