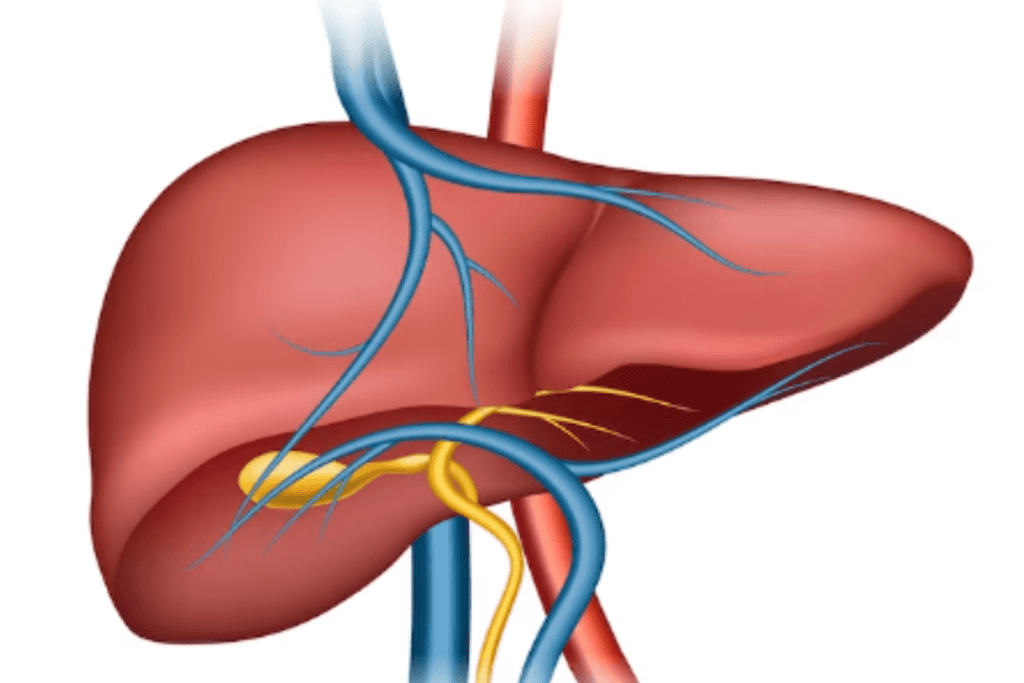
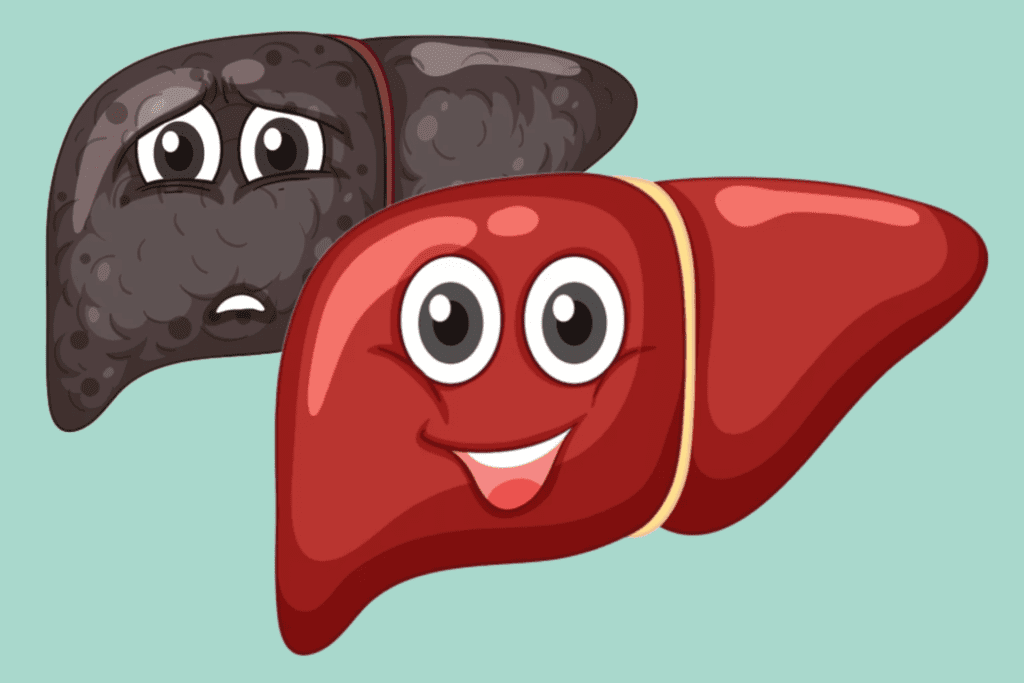
Hepatitis is an inflammatory condition of the liver, often caused by viral infections (hepatitis A, B, C, etc.) or other factors like alcohol consumption, toxins, or autoimmune diseases. It can lead to liver dysfunction and various symptoms, ranging from mild to severe.
Table of Contents
ToggleThis is classified into two main categories:
Classification
Hepatitis can indeed be classified broadly into two main categories:
Viral hepatitis and non-viral hepatitis, based on the underlying causes.
Viral Hepatitis
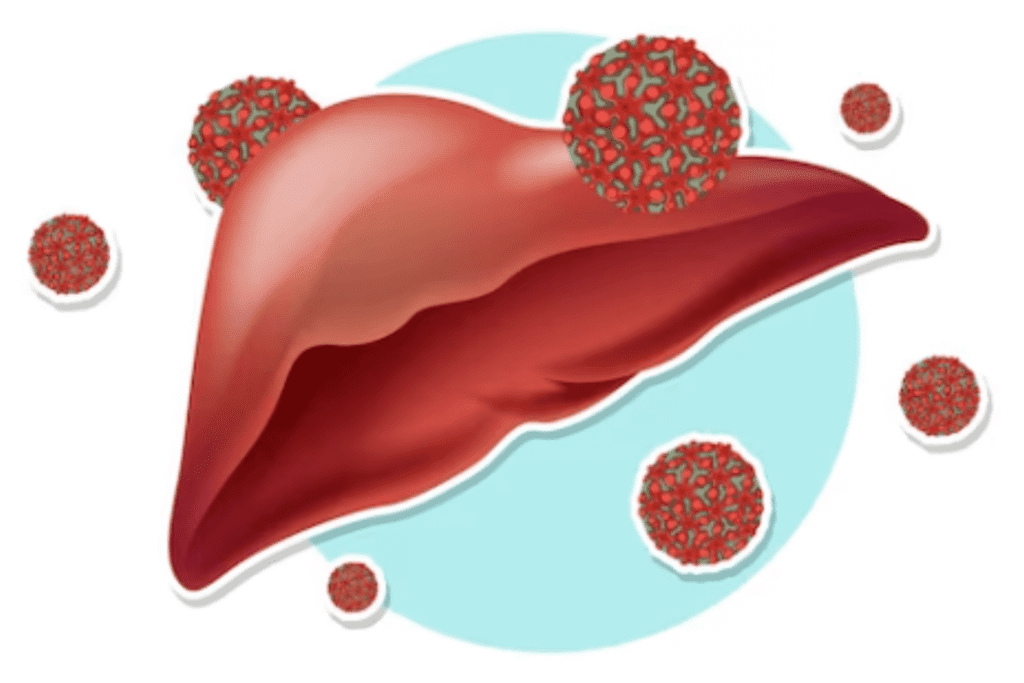
Viral hepatitis is caused by specific hepatitis viruses and is the most common form of hepatitis.
Types
The main types of viral hepatitis are:
- Hepatitis A (HAV)
- B (HBV)
- C (HCV)
- D (HDV) -Only occurs in individuals with HBV
- E (HEV)
- G (HGV)
1. Hepatitis A (HAV)
Symptoms
HAV symptoms typically appear within 2 to 6 weeks after exposure to the virus. The symptoms encompass a broad range from mild to severe, including:
- Fatigue and weakness
- Loss of appetite
- Nausea and vomiting
- Abdominal pain or discomfort, particularly in the region of the liver, may be experienced.
- Dark urine
- Pale or clay-colored stools
- Jaundice (characterized by the yellowing of the skin and eyes, which may be observed)
- Low-grade fever
- Muscle aches
- Itchy skin
Causes
HAV is caused by the hepatitis A virus, primarily transmitted through the fecal-oral route, where contaminated food or water carries the virus from an infected person’s feces to the mouth of another.
The main modes of HAV transmission include:
Consumption of Contaminated Food:
Consuming food, especially fruits, vegetables, or shellfish, contaminated with the virus.
Drinking Contaminated Water:
Drinking water that has been contaminated with the virus
Close Contact with an Infected Person:
Coming into contact with an infected person’s feces through poor hygiene practices, inadequate handwashing, or sexual contact.
Poor Sanitation:
Living in areas with inadequate sanitation facilities can increase the risk of HAV transmission.
Travel to Regions with High HAV Prevalence:
Some regions have higher rates of hepatitis A, and travelers to these areas may be at increased risk of exposure.
Treatment
There is no specific antiviral treatment for HAV as the infection usually resolves on its own over time. Treatment for hepatitis A primarily focuses on supportive care to alleviate symptoms and help the liver recover.
If you have been diagnosed with HAV or suspect you may have the infection, here are some self-care tips to help manage the condition and support your recovery:
Rest:
Get plenty of rest to aid in the healing process and conserve energy for your body to fight the virus.
Hydration:
Drink plenty of fluids, especially water, to stay well-hydrated. This helps your liver function more effectively and prevents dehydration.
Nutrition:
Focus on a well-balanced, nutritious diet. Choose foods that are easy on the liver, such as fruits, vegetables, whole grains, and lean proteins. Refrain from consuming foods that are high in fat, salt, and sugar.
Avoid Alcohol and Certain Medications:
Refrain from consuming alcohol and avoid medications that can be harmful to the liver during this time.
Manage Symptoms:
If you experience symptoms like nausea or itching, work with your healthcare provider to manage them effectively.
Practice Good Hygiene:
Practice thorough handwashing after using the restroom and before eating or preparing food to prevent the spread of the virus to others.
Avoid Close Contact:
As hepatitis A is contagious, avoid close contact with others, especially in crowded environments, until you are no longer infectious.
Stay Home:
If possible, consider taking time off work or school during the acute phase of the illness to rest and prevent the spread of the virus.
Follow Medical Advice:
Adhere to your healthcare provider’s recommendations, attend follow-up appointments, and get necessary blood tests to monitor your liver function.
Vaccination:
After recovering from hepatitis A, consider getting vaccinated to protect yourself from future infections.
2. Hepatitis B (HBV)
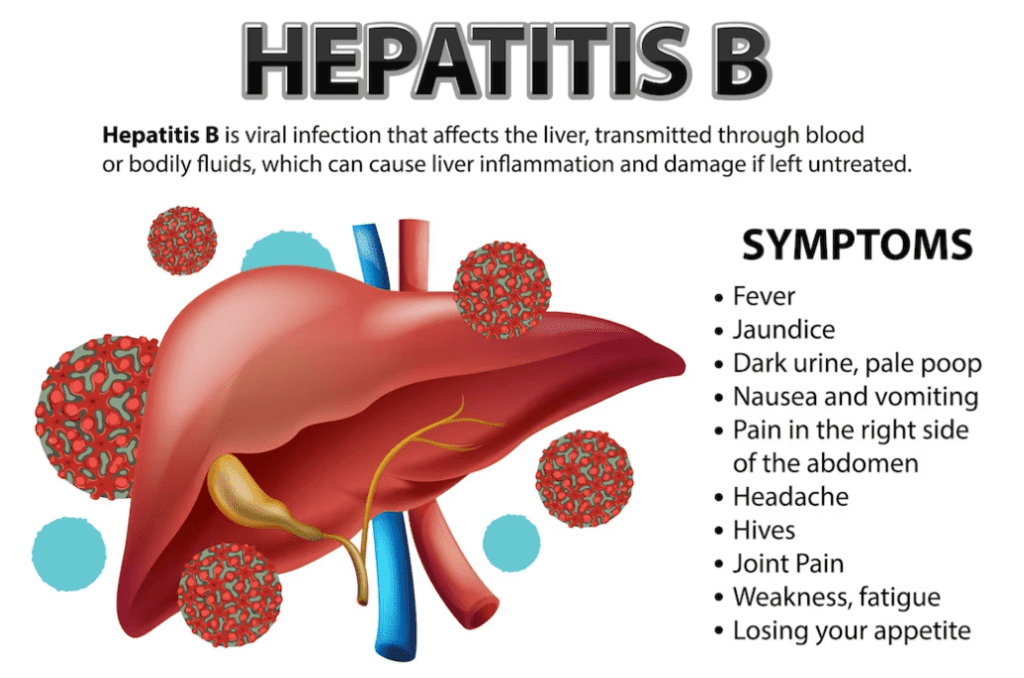
Stages and Symptoms
HBV symptoms can vary depending on the stage of infection and the individual’s immune response. Some people with HBV may experience mild or no symptoms, while others may have more severe manifestations.
The three main stages of hepatitis B infection and their associated symptoms are:
1. Acute HBV:
Acute hepatitis B refers to the initial phase of HBV infection, which typically lasts for a few weeks to several months. During this stage, the immune system recognizes the virus and mounts a response to fight it.
Acute HBV can manifest with a range of symptoms, including:
- Fatigue and weakness
- Loss of appetite
- Nausea and vomiting
- Abdominal pain or discomfort
- Jaundice (The presence of yellowing in the skin and eyes)
- Dark urine
- Pale stools
- Low-grade fever
- Muscle and joint aches
2. Chronic HBV:
Chronic HBV refers to a long-term and persistent infection with HBV. Unlike acute hepatitis B, where the immune system typically clears the virus from the body within a few months, chronic HBV occurs when the virus persists in the body for six months or longer.
- Many individuals with chronic HBV infection may not experience noticeable symptoms for an extended period.
- As the infection progresses, symptoms may include fatigue, jaundice, and complications related to liver damage, such as ascites (fluid buildup in the abdomen) and hepatic encephalopathy (brain dysfunction due to liver failure).
3. Fulminant HBV (Rare, but severe form):
Rapid and severe liver failure leads to life-threatening complications.
It is important to note that some people may carry the HBV virus without showing symptoms, making regular testing and screenings important, especially for individuals at higher risk, such as those born to HBV-infected mothers, healthcare workers, and individuals with multiple sexual partners.
Causes
HBV is caused by the hepatitis B virus, which is a DNA virus belonging to the Hepadnaviridae family. The virus is primarily transmitted through contact with infected bodily fluids.
The main pathways of HBV transmission comprise:
Blood and Body Fluids:
HBV is present in high concentrations in the blood and certain body fluids of infected individuals. It can be transmitted through contact with infected blood, such as through sharing of contaminated needles or syringes, or contact with open sores or wounds.
Sexual Contact:
HBV can be transmitted through unprotected sexual intercourse with an infected partner. It falls under the category of sexually transmitted infections (STIs).
Mother-to-Child Transmission:
During childbirth, an infected mother can transmit the virus to her baby, and the risk of transmission is elevated in cases of maternal chronic infection.
Sharing Personal Items:
Sharing items like razors or toothbrushes with an infected person can also lead to transmission, as these items may have traces of infected blood.
Medical Procedures:
In some cases, HBV transmission can occur through unsafe medical practices, such as using unsterilized or improperly sterilized medical equipment.
Needlestick Injuries:
Healthcare workers and others exposed to accidental needlestick injuries or contact with infected blood are at risk of acquiring HBV.
Dialysis:
Patients undergoing hemodialysis are at risk of exposure to HBV if there is contamination of dialysis equipment.
Tattooing and Piercing:
If proper sterilization procedures are not followed, tattooing and body piercing can also lead to transmission.
Treatment
The treatment of hepatitis B (HBV) aims to suppress the virus, reduce liver inflammation, and prevent the progression of liver damage. The specific treatment approach depends on various factors, including the stage of the infection, the degree of liver damage, and the individual’s overall health.
Below are several commonly used treatment options for HBV:
Antiviral Medications:
Antiviral drugs are used to HBV include entecavir, tenofovir, lamivudine, adefovir, and telbivudine. These drugs can help control the infection and slow down the progression of liver disease.
Interferon Therapy:
Interferon-alpha is an immune-modulating medication that can be used in certain cases of chronic hepatitis B. It helps boost the body’s immune response to the virus. Interferon therapy is typically administered through injections and is used less frequently than antiviral medications due to its side effects and limited effectiveness in some patients.
Liver Function Monitoring:
Regular monitoring of liver function through blood tests is essential to assess the progression of the disease and the effectiveness of treatment.
Liver Cancer Screening:
Individuals with chronic HBV are at an increased risk of developing liver cancer. Therefore, regular screening for liver cancer (e.g., ultrasound and blood tests) is crucial for early detection and timely intervention if necessary.
Lifestyle Modifications:
Embracing a healthy lifestyle can promote liver health. This includes avoiding alcohol, maintaining a balanced diet, exercising regularly, and avoiding substances that may be harmful to the liver.
Immunization:
Vaccination against hepatitis A and hepatitis B is recommended for individuals with chronic hepatitis B to prevent further liver damage from additional infections.
3. Hepatitis C (HCV)
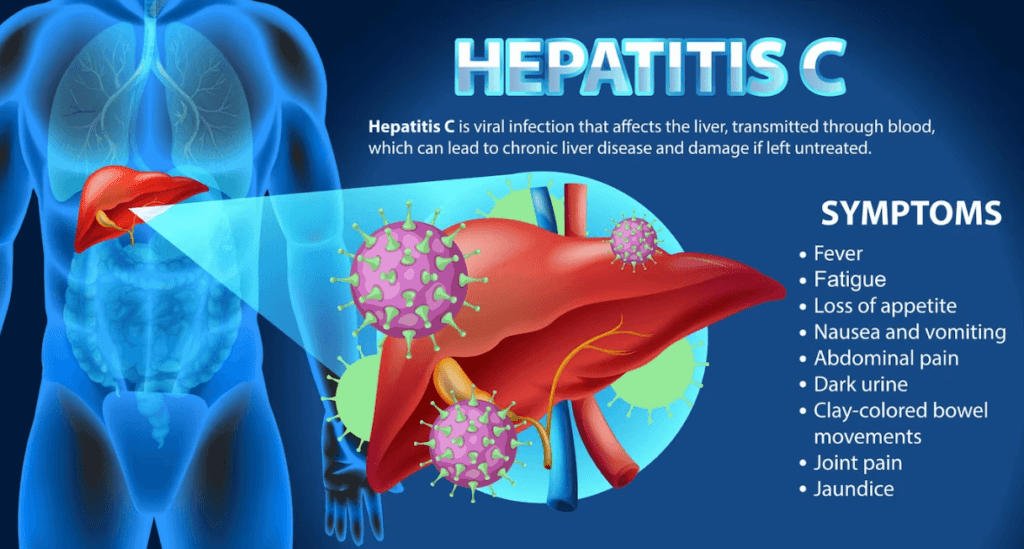
Symptoms
Hepatitis C (HCV) symptoms can vary widely from mild to severe, and some people with the infection may not experience any symptoms at all. If symptoms do occur, they typically appear within 2 to 12 weeks after exposure to the virus.
Common symptoms of acute HCV include:
- Fatigue and Weakness
- Loss of Appetite
- Nausea and Vomiting
- Abdominal Pain
- Jaundice
- Dark Urine
- Pale Stools
- Fever
Causes
HCV is caused by the hepatitis C virus, which is a blood-borne virus belonging to the Flaviviridae family. The main mode of transmission for HCV is through contact with infected blood.
The most common causes of HCV transmission include:
Injecting Drug Use:
Sharing contaminated needles, syringes, or other drug paraphernalia among intravenous drug users is a significant risk factor for HCV transmission.
Blood Transfusions and Organ Transplants:
Before 1992, blood and blood products were not routinely screened for HCV, leading to the transmission of the virus through blood transfusions and organ transplants. Nowadays, strict screening procedures have significantly reduced this risk.
Healthcare-Related Exposures:
Accidental needlestick injuries or contact with contaminated medical equipment can transmit HCV to healthcare workers.
Mother-to-Child Transmission:
Pregnant women with HCV can pass the virus to their babies during childbirth, although the risk is relatively low compared to other types of viral hepatitis.
Unsafe Tattooing and Piercing:
If proper sterilization procedures are not followed, tattooing and body piercing can also lead to HCV transmission.
Sharing Personal Items:
Sharing personal items, such as razors or toothbrushes, that may come into contact with blood can also lead to HCV transmission.
HCV is not spread through casual contact like hugging, kissing, or sharing food and water. It is essential to take preventive measures to avoid HCV transmission, such as not sharing needles, practicing safe sex, and ensuring the use of sterile equipment in medical and tattooing settings.
Currently, there is no vaccine available for hepatitis C, so prevention and early detection are crucial in managing the spread of the virus and reducing its impact on public health.
Treatment
The treatment of hepatitis C (HCV) has evolved significantly in recent years, thanks to the development of direct-acting antiviral (DAA) medications. These antiviral drugs target specific steps of the HCV replication cycle, leading to high cure rates and fewer side effects compared to older treatment regimens. The goals of HCV treatment are to achieve sustained virologic response (SVR), which means undetectable HCV in the blood six months after completing treatment, and to prevent liver damage and complications. The treatment plan may vary based on the HCV genotype, the extent of liver damage (fibrosis or cirrhosis), and the patient’s overall health.
Commonly used DAAs include:
NS5A Inhibitors:
Examples include ledipasvir, velpatasvir, and glecaprevir. They block the NS5A protein, which is essential for viral replication.
NS5B Polymerase Inhibitors:
Examples include sofosbuvir and dasabuvir. They inhibit the NS5B RNA-dependent RNA polymerase, essential for HCV replication.
NS3/4A Protease Inhibitors:
Examples include grazoprevir and glecaprevir. They block the NS3/4A protease enzyme, which is critical for viral replication.
Combination Therapies:
HCV treatment typically involves a combination of two or more DAAs, which are often combined into single-pill regimens for ease of administration.
The duration of treatment can range from 8 to 24 weeks, depending on factors such as HCV genotype, liver health, and prior treatment history. DAAs have high cure rates, typically exceeding 90% across all HCV genotypes.
4. Hepatitis D (HDV)
Symptoms and Causes
Hepatitis D also referred to as delta hepatitis, is a liver infection resulting from the hepatitis D virus (HDV). HDV is an incomplete virus that requires the presence of the hepatitis B virus (HBV) to replicate and cause an infection. Hepatitis D can occur as a co-infection with HBV or as a superinfection in individuals who already have chronic HBV infection.
The symptoms of hepatitis D are similar to those of acute hepatitis B. The symptoms can vary in intensity and may encompass:
- Fatigue and Weakness
- Loss of Appetite
- Nausea and Vomiting
- Abdominal Pain
- Jaundice
- Dark Urine
- Pale Stools
- Low-Grade Fever
In some cases, individuals with HDV may have more severe symptoms compared to those with hepatitis B alone. The progression of the disease can lead to chronic liver disease, including cirrhosis (scarring of the liver), and an increased risk of liver failure and liver cancer.
Treatment
The treatment of hepatitis D (HDV) is challenging because HDV is a defective virus that requires the presence of the hepatitis B virus (HBV) for its replication and survival. As a result, effective treatment of HDV often involves targeting both HDV and HBV to control the infection and reduce liver damage. Here are some treatment options for hepatitis D:
Antiviral Medications:
Antiviral drugs that target HBV and can suppress HBV replication may be used to manage HDV infection. These drugs include:
- Tenofovir disoproxil fumarate (TDF)
- Tenofovir alafenamide (TAF)
- Entecavir
Interferon Therapy:
Interferon alpha, an immune-modulating medication, is the only drug that has shown some effectiveness in treating HDV. Interferon alpha can be used as monotherapy or in combination with antiviral medications.
Combination Therapy:
A combination of interferon alpha and antiviral medications may be prescribed to enhance treatment response and improve outcomes.
5. Hepatitis E (HEV)
Symptoms and Causes
Hepatitis E is caused by the hepatitis E virus (HEV), which is a small, single-stranded RNA virus belonging to the Hepeviridae family. The main mode of transmission for HEV is through the consumption of contaminated food or water. The virus is typically found in the feces of infected individuals or animals, and contamination of food and water sources can occur due to poor sanitation practices.
The symptoms of HEV vary depending on the individual, and some people infected with the virus may not show any symptoms at all. When symptoms do occur, they typically manifest within 2 to 6 weeks after exposure to the virus.
Common symptoms of HEV Include:
- Fatigue and Weakness
- Loss of Appetite
- Nausea and Vomiting
- Abdominal Pain
- Jaundice
- Dark Urine
- Pale Stools
- Low-Grade Fever
The severity of symptoms can range from mild to severe, but in general, hepatitis E is usually self-limiting and resolves on its own without specific medical treatment. However, pregnant women, especially those in their third trimester, and individuals with pre-existing liver disease are at a higher risk of developing severe complications from Hepatitis E.
6. Hepatitis G (HGV)
Symptoms and Causes
Hepatitis G, also known as hepatitis G virus (HGV) or GB virus C (GBV-C), is a relatively recently discovered virus that is classified as a flavivirus. HGV is a blood-borne virus, and its prevalence is relatively low compared to other forms of viral hepatitis. The symptoms and clinical significance of hepatitis G infection are not well-defined, and most infected individuals do not show any symptoms. If symptoms do occur, they are usually mild and non-specific, similar to those of other viral infections.
Common symptoms may include fatigue, mild fever, and loss of appetite.
Causes
Blood-Borne Transmission:
HGV is primarily transmitted through exposure to infected blood or blood products. The most common routes of transmission are through contaminated needles, blood transfusions, and organ transplants.
Mother-to-Child Transmission:
In some cases, HGV can be transmitted from an infected mother to her baby during childbirth or through breastfeeding.
Sexual Transmission:
Although rare, HGV may be transmitted through sexual contact with an infected individual.
Shared Personal Items:
There is a theoretical risk of transmission through sharing personal items like razors or toothbrushes if they come into contact with infected blood. Nevertheless, this method of transmission is regarded as less frequent.
It is important to note that most individuals with HGV have no specific liver-related symptoms, and the infection is often subclinical. Unlike some other forms of viral hepatitis, HGV is not associated with chronic liver disease or significant liver damage.
As HGV is primarily transmitted through blood, prevention measures include avoiding the sharing of needles, practicing safe sex, and ensuring the use of sterile equipment in medical and tattooing settings.
Non-Viral Hepatitis
Types
Non-viral hepatitis refers to liver inflammation not caused by viral infections. There are several types of non-viral hepatitis, each with different underlying causes.
The main types of non-viral hepatitis include:
1. Alcoholic Hepatitis
Caused by excessive and prolonged alcohol consumption, alcoholic hepatitis leads to liver inflammation and damage. It is a form of alcoholic liver disease and can range from mild to severe.
2. Autoimmune Hepatitis
In this condition, the liver cells are attacked by the body’s immune system, causing inflammation and liver damage. The precise cause of autoimmune hepatitis remains not fully understood.
3. Toxic Hepatitis
This type of hepatitis is caused by exposure to certain drugs, medications, industrial chemicals, or herbal supplements that can be toxic to the liver. The liver reacts to these substances, resulting in inflammation.
4. Metabolic Hepatitis
Metabolic hepatitis is associated with metabolic disorders that affect the liver, such as fatty liver disease (non-alcoholic fatty liver disease, NAFLD), which can lead to inflammation and liver damage.
5. Ischemic Hepatitis
Also known as shock liver, this form of hepatitis occurs when there is reduced blood flow to the liver, often due to severe shock or low blood pressure. The lack of oxygen and nutrients can cause liver cell injury.
6. Drug-Induced Hepatitis
Certain medications, including some antibiotics, antifungals, and anti-seizure drugs, can cause drug-induced hepatitis as a side effect.
7. Hereditary Hemochromatosis
This is a genetic disorder that leads to excess iron accumulation in the liver, which can cause inflammation and liver damage over time.
8. Wilson's Disease
A rare genetic disorder that causes copper to accumulate in the liver and other organs, leading to liver inflammation and other complications.
9. Alpha-1 Antitrypsin Deficiency
A genetic disorder that causes a deficiency of alpha-1 antitrypsin protein, leading to liver inflammation and other lung-related issues.
10. Neonatal Hepatitis
Neonatal hepatitis, also known as infantile hepatitis, is a term used to describe liver inflammation that occurs in newborn infants within the first few months of life. It is not a specific diagnosis but rather a group of conditions that can lead to liver inflammation in the early weeks or months after birth. Neonatal hepatitis can be caused by various factors, and identifying the exact cause is essential for appropriate management.
Some common causes of neonatal hepatitis include:
Infections:
Neonatal hepatitis can be triggered by viral, bacterial, or parasitic infections that affect the liver. Common viruses include cytomegalovirus (CMV) and hepatitis viruses (HBV, HCV).
Metabolic Disorders:
Certain metabolic disorders, such as alpha-1 antitrypsin deficiency and neonatal hemochromatosis, can lead to liver inflammation in newborns.
Genetic Disorders:
Some genetic conditions, like Alagille syndrome and progressive familial intrahepatic cholestasis (PFIC), can present with neonatal hepatitis.
Autoimmune Conditions:
Although rare, autoimmune hepatitis can also affect infants and lead to neonatal hepatitis.
Biliary Atresia:
This is a condition in which the bile ducts are abnormally formed or blocked, leading to impaired bile flow and liver inflammation.
Toxic Exposures:
Neonatal hepatitis can occur if the baby is exposed to certain drugs or toxins before or after birth.
Unknown Causes:
In some cases, the exact cause of neonatal hepatitis remains unknown.
Prevention
Preventing hepatitis involves taking certain preventive measures to reduce the risk of infection.
Here are some general strategies to prevent hepatitis:
Vaccination

Vaccination is a crucial preventive measure for certain types of hepatitis. Vaccines are readily available for both hepatitis A and hepatitis B. Getting vaccinated can provide immunity and protect you from these viruses. It is especially important for individuals at higher risk, such as healthcare workers, travelers to areas with high hepatitis prevalence, and individuals with certain medical conditions.
Practice Safe Hygiene
Practicing good hygiene can help prevent the spread of hepatitis viruses. Wash your hands thoroughly with soap and water, especially after using the bathroom, changing diapers, and before eating or handling food.
Safe Food and Water
Be cautious with food and water safety, especially when traveling to regions with inadequate sanitation. Avoid consuming raw or undercooked shellfish and ensure that water for drinking and food preparation is clean and safe.
Safe Sex
Use barrier protection, such as condoms, during sexual intercourse to reduce the risk of transmitting hepatitis viruses, especially hepatitis B and hepatitis C.
Avoid Sharing Needles or Personal Items
Do not share needles, syringes, or any personal items that may come into contact with blood, such as razors or toothbrushes. This is crucial for preventing the transmission of HBV and HCV, which can be transmitted through blood-to-blood contact.
Safe Medical Procedures
Ensure that medical and dental procedures involving injections or other invasive procedures are performed using sterile equipment and under appropriate infection control practices.
Be Cautious with Tattoos and Piercings
If you plan to get a tattoo or body piercing, make sure to choose a reputable and licensed facility that follows proper sterilization procedures to prevent infection.
Screening and Testing
For individuals at risk of HBV or HCV (e.g., those with a history of risky behavior, healthcare workers, and individuals with liver disease), regular screening and testing can help detect infections early and initiate appropriate care.
Pregnancy and Newborn Care
Pregnant women should receive hepatitis B screening during prenatal care. If a pregnant woman is positive for hepatitis B, steps can be taken to protect the newborn from infection at birth.
Proper Disposal of Sharps and Medical Waste
Properly dispose of used needles, syringes, and other medical waste to prevent accidental needlestick injuries and transmission of infections.
By adopting these preventive measures and being aware of the risks, you can reduce the chances of acquiring hepatitis and protect your liver health.
Conclusion
In conclusion, hepatitis is a group of viral and non-viral infections that affect the liver and can lead to significant health consequences. Hepatitis A is a viral infection transmitted through contaminated food and water. While hepatitis B, C, D, and E have distinct modes of transmission, with B and C being the most prevalent and potentially severe. Vaccination is a crucial preventive measure for hepatitis A and B. Non-viral hepatitis can result from factors such as alcohol, autoimmune conditions, toxins, and genetic disorders. Early detection, proper medical care, and lifestyle adjustments are essential for managing hepatitis effectively and preventing complications, emphasizing the importance of public health initiatives and individual responsibility.
Resources
Image Designed by Freepik
References
https://www.ncbi.nlm.nih.gov/books/NBK554549/
https://www.ncbi.nlm.nih.gov/books/NBK551570/
https://www.ncbi.nlm.nih.gov/books/NBK459290/
https://www.niddk.nih.gov/health-information/liver-disease/viral-hepatitis/hepatitis-c
https://www.ncbi.nlm.nih.gov/books/NBK555945/
https://www.niddk.nih.gov/health-information/liver-disease/viral-hepatitis/hepatitis-d#vaccine-d
https://www.niddk.nih.gov/health-information/liver-disease/viral-hepatitis/hepatitis-e
https://www.ncbi.nlm.nih.gov/books/NBK532278/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2739332/
https://medicinetoday.com.au/mt/2022/may/feature-article/nonviral-hepatitis-common-causes-and-their-management