We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
Glycogen Storage Disease (GSD) is a group of rare genetic disorders that affect the body’s ability to break down glycogen, a stored form of glucose (sugar), into glucose for energy. This leads to an abnormal accumulation of glycogen in various tissues, primarily the liver and muscles. The different types of GSD are caused by mutations in different genes, resulting in specific enzyme deficiencies that disrupt the normal glycogen metabolism process. Symptoms can vary widely depending on the type of GSD, but they often include muscle weakness, fatigue, low blood sugar, and liver-related problems. Management typically involves dietary adjustments, medication, and sometimes enzyme replacement therapy to alleviate symptoms and prevent complications.
Table of Contents
ToggleHow Glycogen Storage Disease Can Affect Health
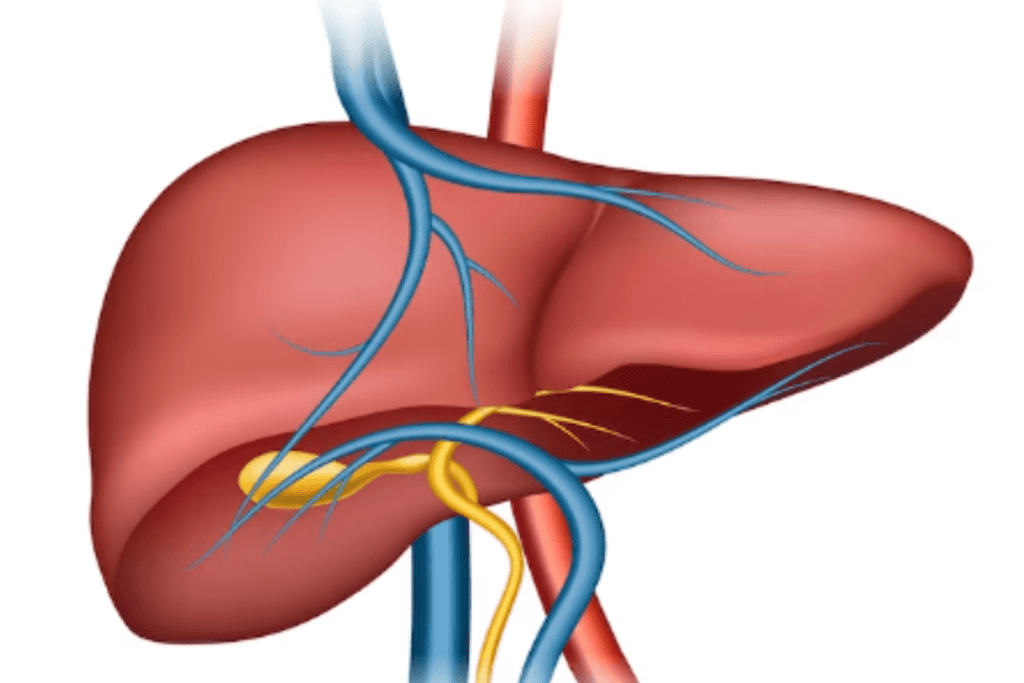
Glycogen storage diseases (GSDs) can have diverse effects on health due to their disruption of glycogen metabolism. Accumulation of excess glycogen in tissues, particularly the liver, and muscles, can lead to symptoms such as muscle weakness, fatigue, low blood sugar (hypoglycemia), and an enlarged liver (hepatomegaly). Depending on the specific type of GSD, other complications might arise, including cardiovascular issues, respiratory problems, and developmental delays.

Types of Glycogen Storage Diseases
There are several types of glycogen storage diseases (GSDs), each caused by a deficiency in a specific enzyme involved in glycogen metabolism.
Here are some of the main types:
GSD Type-0 (von Gierke Disease)
This is characterized by a deficiency of glucose-6-phosphatase, an enzyme responsible for converting glycogen into glucose in the liver. As a result, individuals with GSD-0 have difficulty maintaining normal blood sugar levels and can experience hypoglycemia (low blood sugar).
GSD Type-Ia (von Gierke-Disease)
GSD-Ia is similar to GSD-0 but involves a deficiency in glucose-6-phosphatase translocase, which transports glucose-6-phosphate into the endoplasmic reticulum. This deficiency causes glycogen to accumulate in the liver and kidneys.
GSD Type-Ib
In addition to glycogen accumulation in the liver and kidneys, GSD-Ib affects white blood cells (neutrophils) due to a deficiency in glucose-6-phosphate transporter. This could lead to a higher vulnerability to infections.
GSD Type-II (Pompe Disease)
Pompe Disease is caused by a deficiency of acid alpha-glucosidase, which leads to glycogen buildup in various tissues, especially muscles. It results in progressive muscle weakness, respiratory difficulties, and cardiac issues.
GSD Type-IIIa (Cori Disease)
This disorder involves a deficiency of the debranching enzyme, leading to abnormal glycogen structure in both liver and muscle cells. Symptoms may include hepatomegaly (enlarged liver), muscle weakness, and hypoglycemia.
GSD Type-IIIb (Cori Disease)
GSD-IIIb is a milder form of GSD-III that primarily affects the liver. It shares some characteristics with GSD-IIIa but typically has fewer muscle-related symptoms.
GSD Type-IVa (Andersen Disease)
This disease results from a deficiency of glycogen branching enzyme, causing abnormal glycogen accumulation that affects various organs, leading to severe liver and heart problems.
GSD Type-IVb (Andersen Disease)
GSD-IVb is a milder variant of GSD-IVa, primarily affecting the liver. While it still results in liver issues, it typically has a slower progression compared to GSD-IVa.
GSD Type-V (McArdle Disease)
McArdle Disease is caused by a deficiency of muscle phosphorylase, impairing the breakdown of glycogen in muscles. This leads to exercise intolerance, muscle cramps, and weakness during physical activity.
GSD Type-VI (Hers Disease)
Hers Disease is characterized by a deficiency of liver phosphorylase, causing glycogen accumulation specifically in the liver. It may result in hepatomegaly and fasting hypoglycemia.
GSD Type-VII (Tarui Disease)
Tarui Disease results from a deficiency of muscle phosphofructokinase, impacting the metabolism of glucose in muscles. This leads to exercise intolerance and muscle-related symptoms.
GSD Type-VIII (Phosphorylase b Kinase Deficiency)
GSD-VIII involves a deficiency of phosphorylase b kinase, an enzyme that activates glycogen phosphorylase. Its presentation can vary widely, with symptoms affecting multiple organ systems.
GSD Type-IX
GSD-IX includes several subtypes, each caused by a deficiency in different enzymes involved in glycogen metabolism. The specific symptoms and severity depend on the subtype.
GSD Type-XI (Fanconi-Bickel Syndrome)
Fanconi-Bickel Syndrome is caused by glucose transporter protein deficiency, affecting glucose and galactose transport. This leads to hepatomegaly, renal dysfunction, and other metabolic abnormalities.
What are the Symptoms of Glycogen Storage Disease?
The symptoms of glycogen storage diseases (GSDs) can vary widely depending on the specific type of GSD. However, there are some common symptoms and features that are often observed across various types:
Hypoglycemia (Low Blood Sugar)
Many GSDs lead to episodes of low blood sugar, resulting in symptoms such as fatigue, irritability, dizziness, shakiness, sweating, confusion, and, in severe cases, seizures or loss of consciousness.
Enlarged Liver (Hepatomegaly)
Accumulation of glycogen in the liver can lead to hepatomegaly, causing an enlarged abdomen and discomfort.
Muscle Weakness and Fatigue
GSDs can result in muscle weakness, fatigue, and exercise intolerance due to the inability to effectively utilize stored glycogen for energy.
Exercise Intolerance
Individuals with GSDs may experience limited stamina and discomfort during physical activities due to their reduced ability to break down glycogen for energy.
Muscle Cramps and Pain
Muscle cramps, pain, and discomfort are common, especially during exercise, as the muscle cells struggle to access stored glycogen.
Delayed Growth and Development
Children with GSDs may experience growth delays and developmental issues due to energy limitations affecting normal growth.
Cardiac Symptoms
Some GSDs can lead to cardiac issues, including arrhythmias, cardiomyopathy (enlarged heart), and heart failure.
Respiratory Issues
Certain GSD types can affect the muscles involved in breathing, causing respiratory difficulties, especially during physical activity or sleep.
Joint Problems
Muscle weakness and limitations in physical activity can lead to joint pain and stiffness.
Gastrointestinal Symptoms
Nausea, vomiting, diarrhea, and abdominal discomfort can occur in some GSDs.
Frequent Infections
Immune system dysfunction in certain GSD types can increase susceptibility to infections.
Neurological Symptoms
Some GSDs can affect the nervous system, leading to symptoms such as seizures, cognitive impairments, and developmental delays.
Renal Dysfunction
Certain GSDs, like Fanconi-Bickel Syndrome, can impact kidney function, leading to renal dysfunction.
Bone Health Issues
GSDs can affect bone health, leading to abnormalities like osteoporosis.
Metabolic Crises
Fasting or illness can trigger metabolic crises in GSDs, resulting in severe symptoms and complications due to the lack of available energy.
What Causes Glycogen Storage Disease?
Glycogen storage diseases (GSDs) are primarily caused by genetic mutations that affect the enzymes responsible for glycogen metabolism. These mutations can lead to enzyme deficiencies, which in turn disrupt the normal breakdown, synthesis, or structure of glycogen in the body. Glycogen is a complex carbohydrate that serves as a storage form of glucose, providing energy when needed.
The specific genetic mutations causing GSDs vary depending on the type of GSD. Different types of GSDs are associated with mutations in specific genes that code for enzymes involved in different steps of glycogen metabolism. The mutations can lead to either a lack of the enzyme or a defective enzyme, resulting in abnormal glycogen accumulation or structure in various tissues.
GSDs are typically inherited in an autosomal recessive manner, meaning that an individual needs to inherit two mutated copies of the gene (one from each parent) to develop the disorder. Carriers, who inherit one normal gene and one mutated gene, usually do not exhibit symptoms but can pass the mutated gene to their offspring.
While the underlying cause of GSDs is genetic, the resulting symptoms and complications can be quite diverse depending on the type of GSD and the affected tissues. These symptoms often arise due to the inability of cells to properly break down glycogen into glucose, leading to energy shortages and metabolic imbalances.
How is Glycogen Storage Disease Diagnosed?
The diagnosis of glycogen storage disease (GSD) involves a combination of clinical evaluation, laboratory tests, imaging studies, and genetic testing. Since there are different types of GSDs, each with distinct symptoms and enzyme deficiencies, the diagnostic process can vary.
Here’s an overview of the typical steps involved in diagnosing GSD:
1. Clinical Assessment
A medical professional, often a pediatrician, geneticist, or metabolic specialist, evaluates the patient’s medical history and conducts a thorough physical examination to identify any characteristic symptoms, such as hepatomegaly (enlarged liver), muscle weakness, growth issues, and hypoglycemia.
2. Laboratory Tests
Blood Tests:
Blood samples are analyzed for markers such as glucose, lactate, liver enzymes, creatine kinase, and other metabolic parameters that can indicate abnormal glycogen metabolism.
Urine Tests:
Urine samples may be analyzed to check for the presence of certain metabolites that can be indicative of GSDs.
3. Imaging Studies
Ultrasound or MRI:
Imaging techniques can help visualize the liver and other affected organs, assessing their size and structure.
4. Enzyme Activity Assays
In some cases, enzyme activity assays can help confirm the specific type of GSD. These tests measure the activity levels of enzymes involved in glycogen metabolism.
5. Genetic Testing
Genetic testing is a crucial step in diagnosing GSDs. It involves analyzing the patient’s DNA to identify specific mutations associated with different types of GSDs. This can help confirm the diagnosis and determine the exact subtype of GSD.
6. Muscle Biopsy
In certain cases, a muscle biopsy may be performed to assess the structure and composition of glycogen within muscle tissue. This can provide valuable information about the specific type of GSD.
7. Glucose Tolerance Test
A glucose tolerance test involves administering a controlled amount of glucose and monitoring the body’s response. Abnormal glucose levels or delayed response can indicate GSD.
8. Liver Biopsy
In cases where liver involvement is significant, a liver biopsy may be performed to assess glycogen accumulation and its impact on liver function.
Glycogen Storage Disease Treatment
The treatment of glycogen storage diseases (GSDs) varies depending on the specific type of GSD and the severity of the disease. Since GSDs are caused by enzyme deficiencies affecting glycogen metabolism, treatment aims to manage symptoms, prevent complications, and improve the overall quality of life for affected individuals.
Here are some general approaches to GSD treatment:
Dietary Management
Dietary modifications are often a cornerstone of GSD treatment. The goal is to provide a consistent source of glucose to prevent hypoglycemia and minimize glycogen accumulation. This may involve frequent meals, complex carbohydrates, and avoiding fasting. In some cases, a special medical formula might be prescribed.
Supplemental Nutrition
In certain GSD types, glucose polymers or cornstarch can be ingested before bedtime to provide a sustained release of glucose during the night, helping to prevent hypoglycemia.
Enzyme Replacement Therapy
In some GSD types, especially those affecting the liver, enzyme replacement therapy might be considered to introduce the missing enzyme. However, this approach is limited by challenges such as enzyme stability and delivery to target tissues.
Medications
Medications might be used to manage specific symptoms or complications. For example, medications to manage muscle pain, control seizures, or address cardiac issues may be prescribed depending on the individual’s needs.
Exercise Guidelines
Careful exercise management is important. Regular physical activity can help improve muscle strength and cardiovascular health, but it’s essential to prevent excessive muscle breakdown and hypoglycemia. Working with a medical professional to develop an appropriate exercise plan is crucial.
Genetic Counseling
Genetic counseling is recommended for affected individuals and their families to understand the inheritance pattern, and potential risks for future children, and make informed decisions.
Regular Medical Monitoring
Individuals with GSDs require regular medical follow-up to monitor symptoms, growth, and organ function, and to adjust treatment strategies as needed.
Management of Acute Crises
During illnesses or situations that may impact nutrition intake, individuals with GSDs need careful monitoring and sometimes hospitalization to prevent metabolic crises.
Liver Transplantation
In some severe cases of GSDs affecting the liver, liver transplantation might be considered to provide a functional source of the missing enzyme. This is typically reserved for cases where other treatments have been ineffective or the disease is life-threatening.
Research and Clinical Trials
For some GSD types, ongoing research and clinical trials may offer new treatment options, including experimental therapies.
Conclusion
Glycogen storage diseases (GSDs) are a group of genetic disorders caused by enzyme deficiencies in glycogen metabolism. They lead to symptoms such as hypoglycemia, hepatomegaly, muscle weakness, and growth issues. Diagnosis involves clinical assessment, genetic testing, and imaging. While most GSDs are not curable, treatment strategies aim to manage symptoms and improve quality of life through dietary modifications, enzyme replacement, medications, and more. Early diagnosis and personalized care are crucial. Genetic counseling helps families understand inheritance patterns. Collaboration with specialists is key to effective management. Ongoing research offers hope for advancements in GSD treatment and care.
References
https://www.ncbi.nlm.nih.gov/books/NBK459277/
https://www.ncbi.nlm.nih.gov/books/NBK534196/
https://pubmed.ncbi.nlm.nih.gov/29083788/
https://pubmed.ncbi.nlm.nih.gov/21910565/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7442342/
https://www.archivesofmedicalscience.com/Hepatic-glycogen-storage-diseases-pathogenesis-clinical-symptoms-and-therapeutic,81093,0,2.html
https://www.britannica.com/science/glycogen-storage-disease