We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
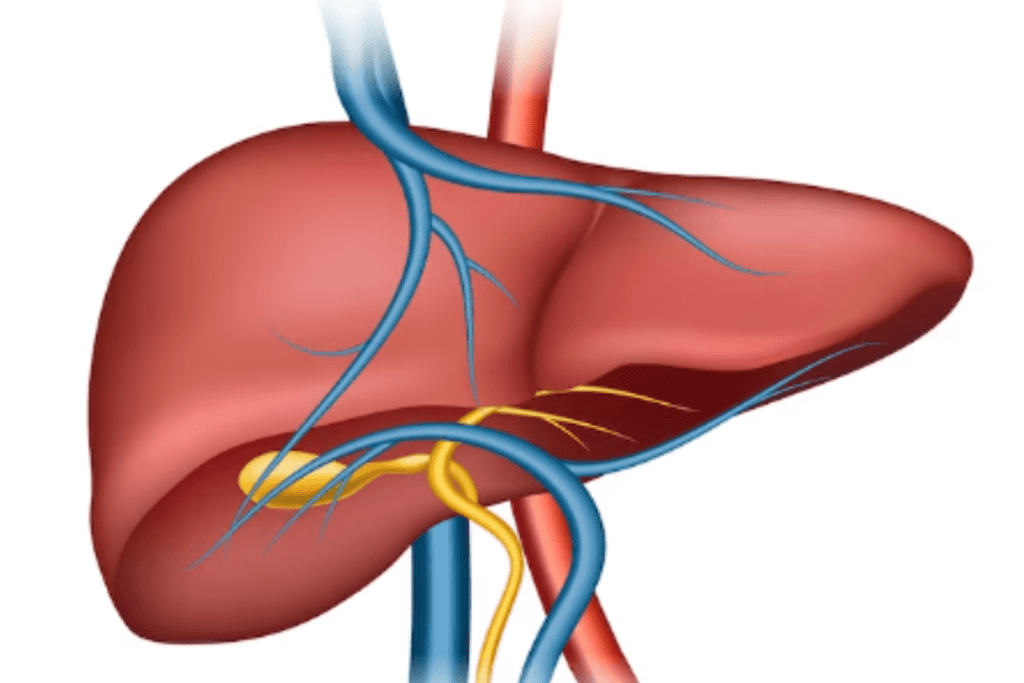
Fatty liver disease is a condition where excess fat accumulates in liver cells. It can result from alcohol consumption or factors like obesity and diabetes. This can lead to inflammation, scarring, and potentially severe liver damage.
Table of Contents
ToggleIs Fatty Liver Dangerous?
Fatty liver can be dangerous if not managed properly. It can lead to inflammation, scarring, and potentially progress to more severe liver conditions, such as cirrhosis and liver failure.
Stages of Fatty Liver Disease
myupchar.com/en, CC BY-SA 4.0, via Wikimedia Commons
Fatty liver disease progresses through several stages, each representing increasing severity of liver damage.
The stages are as follows:
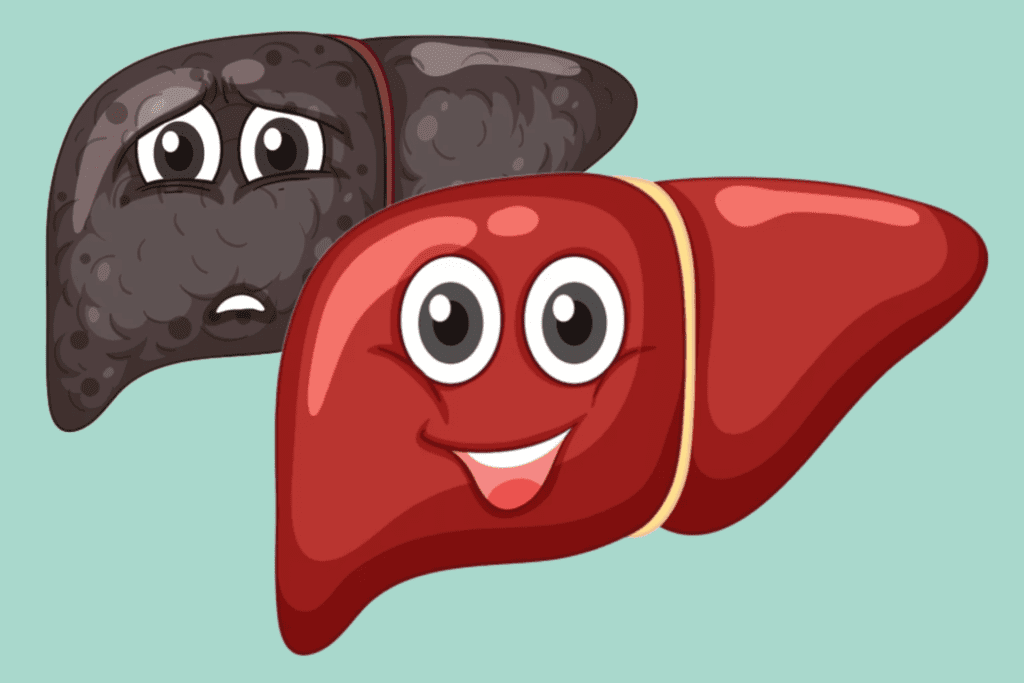
Simple Fatty Liver (Steatosis)
In the initial stage, excess fat accumulates in liver cells, but there is no significant inflammation or cell damage. This stage often has no symptoms and is usually reversible with lifestyle changes.
Non-Alcoholic Steatohepatitis (NASH)
As fat accumulation continues, inflammation and liver cell damage occur. NASH is a more serious stage and can lead to fibrosis. Some individuals with NASH may experience symptoms such as fatigue, abdominal discomfort, or elevated liver enzymes in blood tests.
Fibrosis
Continued inflammation triggers the formation of scar tissue in the liver, known as fibrosis. Fibrosis indicates a progression toward more severe liver damage. The extent of fibrosis can range from mild to advanced.
Cirrhosis
In this advanced stage, extensive scar tissue replaces healthy liver tissue, causing significant impairment of liver function. Cirrhosis can lead to symptoms like jaundice, fluid retention, confusion, and easy bleeding. It increases the risk of liver failure and liver cancer.
Liver Failure and Complications
If cirrhosis becomes severe, the liver’s ability to perform vital functions declines, leading to liver failure. This can result in serious complications such as bleeding disorders, fluid accumulation in the abdomen (ascites), mental confusion (hepatic encephalopathy), and increased susceptibility to infections.
What are the Types of Fatty Liver Disease?
There exist two primary categories of fatty liver disease:
Alcoholic Fatty Liver Disease (AFLD)
Excessive intake of alcohol leads to the development of this form of fatty liver disease. The liver metabolizes alcohol, and chronic alcohol abuse can lead to fat accumulation in liver cells. AFLD can range from simple fatty liver (steatosis) to more severe inflammation and liver damage, known as alcoholic hepatitis.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is characterized by fat accumulation in the liver cells without a significant history of alcohol consumption. It is strongly associated with obesity, insulin resistance, metabolic syndrome, type 2 diabetes, and other metabolic disorders. NAFLD itself can progress from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and potentially liver failure.
Within NAFLD, there are further subtypes based on the severity of inflammation and fibrosis:
Non-Alcoholic Steatohepatitis (NASH):
A more advanced form of NAFLD with inflammation and liver cell damage, which can lead to fibrosis and cirrhosis over time.
Fibrosis and Cirrhosis:
As inflammation continues, scar tissue (fibrosis) can develop, leading to cirrhosis in more severe cases. Cirrhosis is characterized by extensive liver scarring and impaired function.
What are the Symptoms of Fatty Liver Disease?
In its early stages, fatty liver often doesn’t cause noticeable symptoms. However, as the condition progresses, especially in more advanced stages like non-alcoholic steatohepatitis (NASH) and cirrhosis, symptoms can become evident.
Common symptoms and signs of fatty liver disease include:
Fatigue
Experiencing fatigue and diminished vitality despite sufficient rest.
Abdominal Discomfort
Mild to moderate discomfort or pain in the upper right side of the abdomen.
Unexplained Weight Loss
Sudden or gradual weight loss without an apparent reason.
Jaundice
Manifests as a yellowing of the skin and eyes, resulting from compromised liver functionality.
Swelling
Accumulation of fluid in the abdomen (ascites) or legs (edema) due to decreased liver function.
Easy Bruising and Bleeding
Impaired liver function can lead to reduced production of clotting factors, resulting in easy bruising and prolonged bleeding.
Itchy Skin
The buildup of toxins in the body may cause itching.
Dark Urine
Urine may appear darker than usual due to the presence of bilirubin.
Pale Stools
Stools may appear pale or clay-colored due to reduced bile production.
Mental Confusion
In advanced stages like cirrhosis, toxins that the liver normally processes can build up in the blood and affect brain function, leading to confusion and difficulty concentrating (hepatic encephalopathy).
What Causes Fatty Liver Disease?
Fatty liver can be caused by several factors, and the underlying mechanisms can vary between different types of the disease.
The main causes are:
Alcohol Consumption
Excessive and chronic alcohol consumption is a primary cause of alcoholic fatty liver disease (AFLD). The liver metabolizes alcohol, and over time, this process can lead to fat accumulation in liver cells and inflammation.
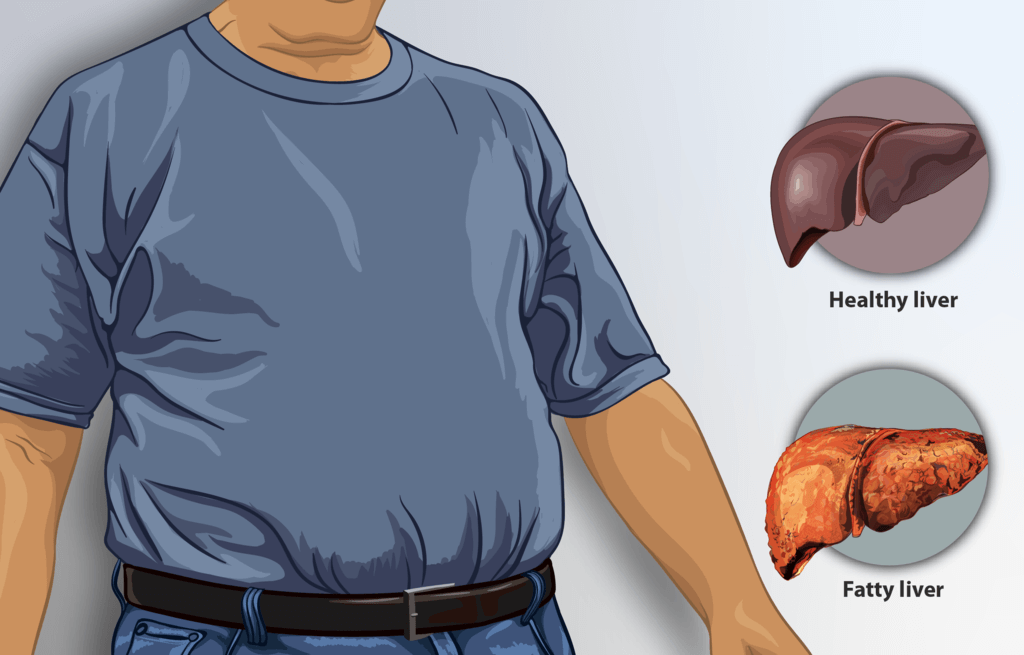
Obesity and Metabolic Factors
Non-alcoholic fatty liver disease (NAFLD) is closely linked to obesity, insulin resistance, metabolic syndrome, and type 2 diabetes. Insulin resistance leads to increased fat storage in the liver.
Dietary Factors
Consuming a diet high in refined sugars, unhealthy fats, and processed foods can contribute to fat buildup in the liver.
Rapid Weight Loss
Rapid weight loss, particularly through crash diets or extreme calorie restriction, can lead to the release of stored fats, overwhelming the liver’s capacity to process them.
Genetics
Genetic factors can influence how the body processes and stores fat, increasing the risk of fatty liver disease in some individuals.
Medications
Certain medications, such as corticosteroids, tamoxifen, and some antiviral drugs, can contribute to the development of fatty liver disease.
Insulin Resistance and Diabetes
Elevated insulin levels can promote fat storage in the liver. People with type 2 diabetes or prediabetes are at a higher risk of NAFLD.
Hepatitis C
Chronic infection with hepatitis C virus (HCV) can lead to fat accumulation in the liver, contributing to the development of fatty liver disease.
Malnutrition
Poor nutrition, including deficiencies in essential nutrients, can affect liver function and contribute to fat buildup.
Other Health Conditions
Certain health conditions, such as polycystic ovary syndrome (PCOS), hypothyroidism, and Wilson’s disease, can increase the risk of fatty liver disease.
How is Fatty Liver Disease Diagnosed?
Fatty liver disease is typically diagnosed through a combination of medical history, physical examination, and various diagnostic tests.
The process may involve the following steps:
Medical History and Physical Examination
Your healthcare provider will ask about your medical history, including alcohol consumption, diet, and any existing health conditions. They will also conduct a physical examination to assess your overall health and check for signs of liver enlargement or tenderness.
Blood Tests
Blood tests are performed to assess liver function and detect markers of liver damage. Common blood tests include liver enzyme tests (ALT, AST), which can be elevated in the presence of liver inflammation or damage, and other markers such as gamma-glutamyl transferase (GGT), alkaline phosphatase, and bilirubin.
Imaging Studies
Ultrasound :
An abdominal ultrasound can reveal the presence of excess fat in the liver and assess its size and structure.
CT Scan or MRI:
These imaging techniques provide more detailed views of the liver and can help assess the extent of fatty infiltration and the presence of complications like cirrhosis.
Fibrosis Assessment
If fatty liver disease is suspected to have progressed to a more advanced stage, additional tests may be done to assess the extent of liver fibrosis. These tests include transient elastography (FibroScan) or specialized blood tests that estimate fibrosis levels.
Liver Biopsy (in some cases)
A liver biopsy involves taking a small sample of liver tissue for microscopic examination. It provides detailed information about the extent of liver damage, inflammation, and fibrosis. However, biopsies are invasive and are often reserved for cases where the diagnosis is unclear or when advanced liver disease is suspected.
Non-Invasive Tests
In recent years, non-invasive methods for assessing liver fibrosis have become more prevalent. These include transient elastography (FibroScan), magnetic resonance elastography (MRE), and specialized blood tests (such as FibroTest or APRI score).
Evaluation of Underlying Causes
If non-alcoholic fatty liver disease (NAFLD) is diagnosed, your healthcare provider may also assess for underlying conditions like obesity, diabetes, and metabolic syndrome, as these factors play a crucial role in disease progression.
How is Fatty Liver Disease Treated?
The treatment approach for fatty liver disease involves a combination of lifestyle modifications, medical management, and addressing underlying conditions. The goals are to reduce fat accumulation in the liver, manage inflammation, and prevent or slow down the progression of the disease.
Here are the primary components of the treatment:
Lifestyle Changes
Weight Loss:
Achieving and maintaining a healthy weight is crucial for managing fatty liver disease. Gradual weight loss through a balanced diet and regular exercise can improve insulin sensitivity and reduce fat accumulation in the liver.
Dietary Modifications :
Emphasize a well-rounded diet comprising whole grains, lean proteins, fruits, vegetables, and beneficial fats. Restrict intake of added sugars, saturated and trans fats, as well as processed foods.
Physical Activity:
Regular exercise, such as aerobic activities and strength training, can help improve insulin sensitivity and promote weight loss.
Avoid Alcohol
For individuals with alcoholic fatty liver disease (AFLD), complete abstinence from alcohol is essential to prevent further liver damage.
Medical Management
Antioxidant Supplements:
Some antioxidants like vitamin E may be recommended by healthcare professionals for certain individuals with non-alcoholic steatohepatitis (NASH), but this should be done under medical supervision.
Medications:
In some cases, medications may be prescribed to manage specific aspects of fatty liver disease, such as diabetes, high cholesterol, or other related conditions.
Treatment of Underlying Conditions
Diabetes Management
Effective management of diabetes, if present, is important to reduce insulin resistance and control blood sugar levels.
High Cholesterol and Blood Pressure Control
Treating high cholesterol and hypertension can help improve overall cardiovascular health and may have positive effects on fatty liver disease.
Regular Monitoring and Follow-Up
Regular medical check-ups and monitoring of liver function through blood tests and imaging studies are essential to track the progression of the disease and make necessary adjustments to the treatment plan.
Advanced Cases and Complications
In advanced cases, where fibrosis or cirrhosis has developed, more specialized medical care may be required. This could include the management of complications like ascites, hepatic encephalopathy, and variceal bleeding.
In some instances, liver transplantation might be considered for individuals with end-stage liver disease.
Who is at Risk for Fatty Liver Disease?
Numerous elements can elevate the likelihood of developing fatty liver disease. It’s important to note that anyone can develop this condition, but certain groups are more susceptible.
Risk factors include:
Obesity
Excess body weight, particularly abdominal obesity, is a significant risk factor for fatty liver disease. Fat accumulation around the abdomen is strongly associated with insulin resistance and metabolic disturbances that contribute to liver fat buildup.
Type 2 Diabetes
Insulin resistance and high blood sugar levels in type 2 diabetes can lead to fat accumulation in the liver. The presence of diabetes increases the risk of non-alcoholic fatty liver disease (NAFLD) and its progression.
Metabolic Syndrome
This cluster of conditions, including obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, increases the risk of NAFLD.
Poor Diet
Consuming a diet high in sugars, unhealthy fats, and processed foods can contribute to the development of fatty liver disease.
Excessive Alcohol Consumption
Chronic alcohol abuse is a leading cause of alcoholic fatty liver disease (AFLD). Even moderate alcohol consumption can contribute to liver fat accumulation in susceptible individuals.
Rapid Weight Loss
Losing weight too quickly, especially through crash diets or extreme calorie restriction, can lead to the release of stored fats, overwhelming the liver’s ability to process them.
Genetics
Genetic factors can influence how the body processes and stores fat, affecting the risk of fatty liver disease.
Polycystic Ovary Syndrome (PCOS)
Women with PCOS, a hormonal disorder, are at an increased risk of developing fatty liver disease due to insulin resistance.
Certain Medications
Some medications, such as corticosteroids, tamoxifen, and antiviral drugs, can contribute to the development of fatty liver.
Hepatitis C Infection
Chronic infection with hepatitis C virus (HCV) can lead to fat accumulation in the liver, increasing the risk of fatty liver disease.
Age
The risk of fatty liver disease increases with age, particularly after age 50.
Ethnicity
Some ethnic groups, such as Hispanics, have a higher prevalence of fatty liver disease.
Other Health Conditions
Certain conditions, including hypothyroidism, sleep apnea, and Wilson’s disease, can increase the risk of fatty liver disease.
Is Fatty Liver Reversible?
Fatty liver disease can be reversible, particularly in its early stages. Lifestyle changes like weight loss, balanced diet, exercise, and limited alcohol intake can reduce liver fat and improve overall health.
Medical management and controlling underlying conditions, such as diabetes and high cholesterol, further aid reversal. The extent of reversibility depends on factors like disease stage and individual commitment.
Early intervention and ongoing monitoring are vital for successful management. While advanced stages like cirrhosis might be less reversible, timely action and sustained efforts can often lead to improved liver health and potentially reverse fatty liver disease’s effects.
How Can Fatty Liver Disease be Prevented?
Fatty liver disease can often be prevented through proactive measures that promote liver health and address risk factors.
Here’s how:
Maintain a Healthy Weight
Aim for a balanced diet and regular physical activity to achieve and maintain a healthy weight. Weight loss can reduce fat accumulation in the liver.
Healthy Eating Habits
Incorporate a diet abundant in whole grains, lean proteins, fruits, vegetables, and beneficial fats. Minimize consumption of processed foods, added sugars, and detrimental fats.
Regular Exercise
Engage in regular physical activity, including both aerobic exercises and strength training, to improve metabolic health and reduce liver fat.
Limit Alcohol Consumption
If you opt to consume alcohol, do it in moderation.
Manage Diabetes
Control blood sugar levels if you have diabetes, as high blood sugar contributes to fat buildup in the liver.
Manage Cholesterol and Blood Pressure
Keep cholesterol and blood pressure levels under control through diet, exercise, and medication if needed.
Avoid Rapid Weight Loss
Gradual weight loss through sustainable methods is preferable to rapid crash diets.
Stay Hydrated
Drink plenty of water to support overall health, including liver function.
Limit Processed Foods
Reduce consumption of highly processed and sugary foods, as they can contribute to fat accumulation.
Avoid Smoking
Smoking can worsen liver health, so quitting or avoiding smoking is beneficial.
Regular Medical Check-Ups
Undergo regular health check-ups to monitor liver function and address risk factors.
Manage Underlying Conditions
Properly manage conditions like diabetes, metabolic syndrome, and obesity to reduce the risk of fatty liver disease.
Medication Review
Consult a healthcare provider to review medications and ensure they don’t contribute to liver damage.
Moderate Caffeine Intake
Some studies suggest that moderate caffeine intake may have protective effects on the liver.
Stay Informed
Educate yourself about fatty liver disease and its risk factors to make informed decisions about your lifestyle.
Diet Tips for Fatty Liver Disease
Maintaining a nutritious diet significantly contributes to the management and prevention of fatty liver disease.
Here’s a dietary approach that can help improve liver health:
Choose Whole Grains
Choose whole grains such as brown rice, quinoa, whole wheat, and oats over refined grains. These options offer fiber and essential nutrients that promote the well-being of the liver.
Prioritize Lean Proteins
Include lean protein sources like poultry, fish, beans, lentils, tofu, and low-fat dairy. Protein helps repair and maintain liver cells.
Increase Fiber Intake
Fiber-rich foods like fruits, vegetables, legumes, and whole grains can help control blood sugar levels and support digestion.
Embrace Healthy Fats
Consume sources of healthy fats such as avocados, nuts, seeds, olive oil, and fatty fish. Omega-3 fatty acids have anti-inflammatory properties.
Minimize Added Sugars
Avoid sugary beverages, candies, and processed snacks. Read labels to identify hidden sugars in packaged foods.
Limit Saturated and Trans Fats
Reduce consumption of fried foods, processed meats, and commercially baked goods that are high in unhealthy fats.
Watch Portion Sizes
Control portion sizes to avoid overeating and excess calorie consumption.
Stay Hydrated
Drink plenty of water throughout the day to help the liver flush out toxins.
Cut Back on Salt
Lower sodium intake to help prevent fluid retention and support cardiovascular health.
Cook at Home
Preparing meals at home gives you control over ingredients and cooking methods.
Eat Regular Meals
Aim for balanced meals with a combination of carbohydrates, protein, and healthy fats. Avoid prolonged periods of fasting.
Reduce Processed Foods
Minimize processed and packaged foods that often contain unhealthy additives, sugars, and fats.
Choose Colorful Produce
Include a variety of colorful fruits and vegetables to provide antioxidants and nutrients that promote liver health.
Limit Alcohol
If you have alcoholic fatty liver disease (AFLD), it’s essential to completely avoid alcohol.
Conclusion
Fatty liver disease, characterized by fat accumulation in liver cells, poses significant health risks. It has two main types: alcoholic and non-alcoholic (NAFLD), with obesity and metabolic factors contributing to NAFLD. While often asymptomatic in early stages, its progression can lead to inflammation, fibrosis, cirrhosis, and liver failure.
Preventive measures include maintaining a healthy weight, balanced diet, exercise, limiting alcohol, and managing underlying conditions like diabetes. Reversibility is possible through lifestyle changes and medical management, especially in the early stages. Regular monitoring, early detection, and personalized care are pivotal for preserving liver health and overall well-being.
References
https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/definition-facts
https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/treatment
https://medlineplus.gov/fattyliverdisease.html
https://www.health.harvard.edu/blog/fatty-liver-disease-what-it-is-and-what-to-do-about-it-2019011015746
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-017-0806-8
https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/eating-diet-nutrition
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342568/