We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
TMJ disorder, or temporomandibular joint disorder, is a condition characterized by dysfunction and discomfort in the temporomandibular joint, which connects the jawbone to the skull. It involves a range of problems affecting the joint, associated muscles, and surrounding structures.
Table of Contents
ToggleWhat is TMJ Dysfunction?
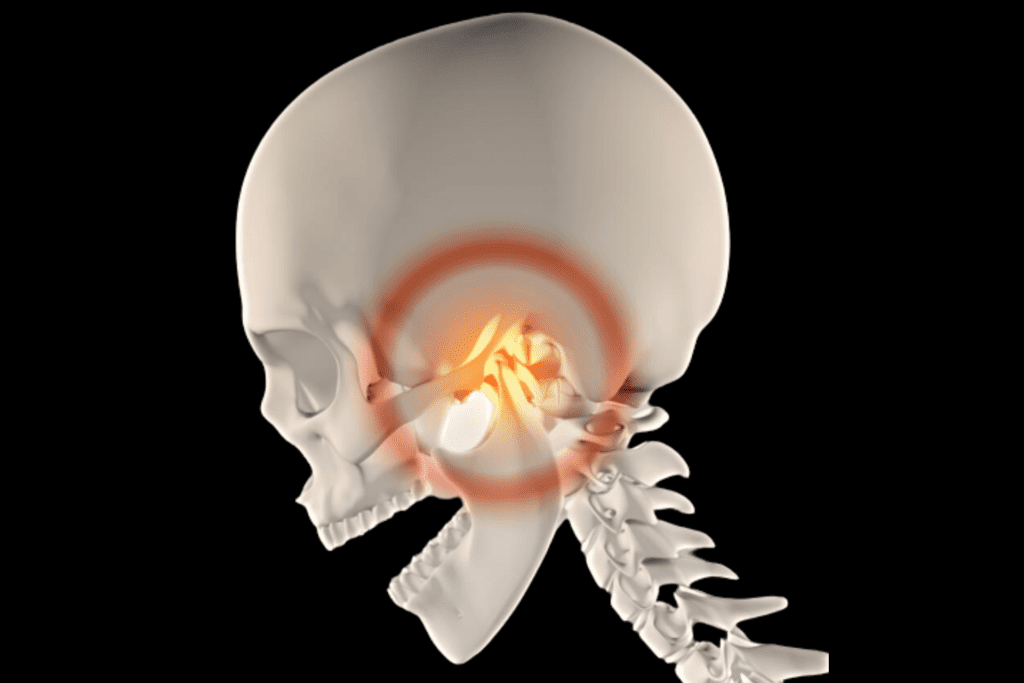
TMJ dysfunction refers to a condition characterized by problems with the functioning of the temporomandibular joint (TMJ) and its associated muscles. It encompasses a range of issues that can affect the jaw joint, resulting in pain, discomfort, and restricted movement. TMJ dysfunction may manifest as jaw pain, clicking or popping sounds, difficulty opening or closing the mouth, headaches, earaches, and facial pain.
Types of TMJ Disorder
TMJ disorder, or temporomandibular joint disorder, can be classified into three main types:
1. Myofascial Pain
Myofascial pain is a prevalent form of temporomandibular joint (TMJ) disorder, which is characterized by distress and discomfort in the muscles responsible for jaw movement. It typically arises due to muscle tension, the presence of trigger points, or excessive strain on the jaw muscles. Common symptoms of myofascial pain include jaw pain, tenderness in the muscles, and difficulties in both opening and closing the mouth.
2. Internal Derangement
Internal derangement refers to structural problems within the temporomandibular joint itself. This can include a displaced disc, dislocated jaw, or misalignment of the joint components. It can result in symptoms such as clicking, popping, or locking of the jaw, as well as pain and restricted jaw movement.
3. Degenerative Joint Disease
Also known as osteoarthritis of the temporomandibular joint, this type involves the progressive deterioration of the joint cartilage. It can occur due to aging, joint overuse, or other factors. Symptoms may include joint stiffness, pain, swelling, and limited jaw movement.
Symptoms TMJ Disorder
TMJ disorder, or temporomandibular joint disorder, can present with a variety of symptoms that affect the jaw joint and surrounding areas. These symptoms may include:
Jaw Pain or Discomfort
TMJ disorder often presents with pain or discomfort in the jaw joint area. This pain can be dull, aching, or sharp and may be present on one or both sides of the jaw. It can range from mild to severe and may worsen with jaw movement or chewing.
Jaw Clicking or Popping
Many individuals with TMJ disorder experience a clicking, popping, or grating sound when they open or close their mouths. This sound is typically caused by the movement of the jaw joint components, such as the disc or condyle, and may or may not be accompanied by pain.
Limited Jaw Movement
TMJ disorder can result in a limited range of motion in the jaw joint. This can make it difficult to fully open or close the mouth, leading to a sensation of jaw stiffness or tightness. In some cases, the jaw may even get stuck in an open or closed position temporarily.
Muscle Stiffness or Tenderness
The muscles surrounding the jaw joint, including the muscles of the face, temples, and neck, can become tight, sore, or tender. This muscle stiffness can cause discomfort, pain, or aching sensations in these areas. Muscle spasms or knots may also be present.
Headaches or Migraines

TMJ disorder can contribute to recurring headaches, which are often described as tension-type headaches or migraines. The pain may be felt in the temples, forehead, or behind the eyes. These headaches may be associated with jaw muscle tension or referred pain from the jaw joint.
Ear-Related Symptoms
TMJ disorder can cause various symptoms related to the ears. These may include earaches, a feeling of fullness or pressure in the ears, or even tinnitus (ringing or buzzing sounds in the ears). Some individuals may experience temporary hearing loss or changes in their ability to hear.
Facial Pain
TMJ disorder can lead to facial pain, typically felt as a dull ache or throbbing sensation in the cheeks, jawline, or temples. The pain may be intermittent or constant and can be aggravated by jaw movements or chewing.
Teeth-Related Symptoms
TMJ disorder can manifest as teeth-related symptoms. This may include unexplained toothaches, tooth sensitivity, or discomfort when biting or chewing. Misalignment of the jaw can affect the way the teeth come together, leading to an uncomfortable bite.
Related: Tooth Pain (Toothache): Overview
TMJ Disorder-Causes

The exact causes of TMJ disorder, or temporomandibular joint disorder, can be multifactorial and may vary among individuals. Some common factors that can contribute to the development of TMJ disorder include:
Jaw Misalignment
If there is a misalignment or imbalance between the upper and lower jaw, it can put a strain on the temporomandibular joint. This can be due to factors like genetics, abnormal jaw development, or prior dental treatments that didn’t address the alignment issue properly.
Teeth Grinding or Clenching (Bruxism)
Bruxism is a common habit of grinding or clenching the teeth, often during sleep or times of stress. The constant pressure and friction on the jaw joint can lead to TMJ disorder. Bruxism can be caused by stress, anxiety, sleep disorders, or certain medications.
Injury or Trauma
A direct injury or trauma to the jaw, face, or temporomandibular joint can damage the joint structures and contribute to TMJ disorder. This can occur due to accidents, sports injuries, physical altercations, or surgical procedures involving the jaw.
Arthritis
Different forms of arthritis, such as osteoarthritis (wear and tear of joint cartilage) or rheumatoid arthritis (an autoimmune disorder), can affect the temporomandibular joint. Inflammation and joint damage from arthritis can lead to TMJ disorder symptoms.
Stress and Muscle Tension
High levels of stress, anxiety, or emotional tension can cause individuals to unknowingly clench their jaw or tighten their facial muscles. This chronic muscle tension in the jaw area can strain the joint and contribute to TMJ disorder.
Hormonal Factors
Hormonal changes, such as those occurring during pregnancy or with the use of hormonal contraceptives, have been associated with an increased risk of developing TMJ disorder. Hormonal fluctuations can affect joint laxity and increase muscle tension in the jaw area.
Malocclusion
Malocclusion refers to dental or bite alignment issues, such as an overbite (upper teeth overlap lower teeth) or an underbite (lower teeth protrude beyond upper teeth). These misalignments can put extra stress on the jaw joint and contribute to TMJ disorder symptoms.
Treatments Of TMJ Dysfunction

Healthcare providers can employ various treatment approaches for TMJ dysfunction, depending on the severity of symptoms and underlying causes. Here are some common treatment options:
1. Nonsurgical TMJ treatments
Nonsurgical treatments are often the first line of approach for managing TMJ dysfunction. Here are some common nonsurgical treatment options:
Self-Care and Lifestyle Modifications:
Self-care practices play a crucial role in managing TMJ dysfunction. It involves adopting habits such as avoiding hard or chewy foods that can strain the jaw joint, practicing stress reduction techniques (such as deep breathing, meditation, or yoga) to minimize jaw clenching, maintaining good posture to alleviate strain on the jaw, and applying heat or cold packs to the affected area to reduce pain and inflammation.
Medications:
Over-the-counter pain relievers like nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation associated with TMJ dysfunction. NSAIDs such as ibuprofen or naproxen are commonly recommended. In some cases, healthcare providers may prescribe stronger pain medications, muscle relaxants, or low-dose tricyclic antidepressants to manage more severe pain or muscle tension.
Oral Appliances:
Dental splints or bite guards are custom-made oral appliances that can be worn over the teeth to alleviate TMJ symptoms. These devices help improve bite alignment, reduce clenching or grinding, and provide stability to the jaw joint. They are typically prescribed and fitted by dentists specializing in TMJ disorders.
Physical Therapy:
Physical therapy for TMJ dysfunction focuses on exercises, stretches, and manual therapy techniques to improve jaw mobility, reduce muscle tension, and enhance overall jaw function. Physical therapists may employ techniques such as jaw exercises, gentle stretches, massage, or ultrasound therapy to alleviate pain and improve muscle strength and flexibility. They may also provide education on posture correction and body mechanics to prevent exacerbation of symptoms.
Stress Management Techniques:
Since stress and tension can contribute to TMJ dysfunction, stress management techniques are beneficial in managing symptoms. These techniques may include relaxation exercises (such as deep breathing or progressive muscle relaxation), mindfulness-based stress reduction, biofeedback (to become aware of muscle tension and learn to relax those muscles), counseling, or referral to a mental health professional for additional support.
Related: What is Stress: How to Manage It?
Transcutaneous Electrical Nerve Stimulation (TENS):
TENS therapy involves the use of low-level electrical currents applied to the jaw muscles to relieve pain and reduce muscle tension associated with TMJ dysfunction. The electrical stimulation helps relax the muscles, increases blood flow, and promotes healing. TENS therapy is typically performed by healthcare professionals trained in TMJ disorders.
Trigger Point Injections:
In some cases, trigger point injections may be used to provide temporary relief from muscle pain and tension associated with TMJ dysfunction. A healthcare provider injects a local anesthetic or a combination of anesthetic and steroid directly into tender or trigger points in the jaw muscles to alleviate pain and reduce muscle spasms.
Laser Therapy:
Low-level laser therapy (LLLT) involves the use of specific wavelengths of light to stimulate healing, reduce inflammation, and alleviate pain associated with TMJ dysfunction. The laser is applied externally to the affected area, and the light energy promotes cellular repair and reduces pain and inflammation. LLLT can be performed by healthcare professionals trained in laser therapy.
2. Surgical TMJ Treatments

Surgical treatments for TMJ dysfunction are typically considered when conservative approaches have not provided sufficient relief or if there are structural issues within the temporomandibular joint that require surgical intervention. Here are some common surgical treatment options for TMJ dysfunction:
Arthroscopy:
Arthroscopy is a minimally invasive surgical procedure that involves inserting a small, thin tube called an arthroscope into the joint space. This allows the surgeon to visualize and assess the condition of the joint structures. Arthroscopy can be used to remove damaged tissue, repair or reposition the disc, or smooth rough joint surfaces. It generally has shorter recovery times compared to open surgery.
Open Joint Surgery:
In cases where more extensive intervention is required, open joint surgery may be performed. This involves making a larger incision to access the joint directly. Open joint surgery allows the surgeon to address complex issues such as joint reconstruction, disc repositioning or replacement, bone grafting, or removal of tumors or cysts within the joint.
Joint Replacement:
Total joint replacement involves replacing the damaged joint surfaces with artificial components made of materials such as metal, plastic, or ceramic. This procedure is typically considered for severe cases of TMJ dysfunction that have not responded to other treatments. Joint replacement can help alleviate pain, improve joint function, and restore oral function.
Joint Restructuring or Repositioning:
In some cases, the jaw joint may require restructuring or repositioning to correct abnormalities or improve alignment. This can involve reshaping the joint components, adjusting the bite relationship, or repositioning the disc to restore proper joint function
Home Treatment and Prevention

Several home treatment strategies can help manage TMJ (temporomandibular joint) dysfunction and alleviate symptoms. Here are a few home remedies you can experiment with:
Apply Moist Heat or Cold Packs
Applying a moist heat pack or a cold compress to the affected jaw area can help reduce pain and inflammation. Use a warm, damp towel or a gel pack wrapped in a thin cloth for heat therapy. For cold therapy, use an ice pack wrapped in a thin towel. As needed, apply for 15-20 minutes multiple times a day.
Practice Jaw Relaxation Exercises
Gentle jaw exercises can help relax the jaw muscles and improve jaw mobility. These exercises may include opening and closing the mouth slowly, side-to-side movements, and gentle stretching exercises. Consult with a healthcare professional or physical therapist for appropriate exercises tailored to your condition.
Eat Soft Foods
Stick to a soft food diet to reduce stress on the jaw joint and muscles. Opt for foods like mashed potatoes, smoothies, soups, yogurt, steamed vegetables, and soft fruits. Avoid hard, chewy, or sticky foods that can exacerbate symptoms.
Avoid Extreme Jaw Movements
Minimize activities that involve excessive jaw movements, such as wide yawning, loud singing, or prolonged wide-mouthed chewing. Be mindful of habits like gum chewing, nail-biting, or clenching the jaw, as these can worsen TMJ symptoms.
Maintain Good Posture
Poor posture can strain the muscles and joints around the jaw. Practice proper posture by keeping your head aligned with your spine, and shoulders relaxed and avoiding forward head posture.
Reduce Stress
Stress can contribute to TMJ symptoms. Engage in stress reduction techniques such as deep breathing, meditation, yoga, or engaging in hobbies and activities that promote relaxation.
Over-the-Counter Pain Relief
To alleviate pain and inflammation associated with TMJ dysfunction, nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can be beneficial. It is important to adhere to the recommended dosage instructions and, if you have any underlying health conditions or are currently taking other medications, consult with a healthcare professional for guidance.
Avoid Excessive Jaw Clenching
Be conscious of jaw-clenching or teeth-grinding habits, particularly during stressful situations or while sleeping. If you notice clenching or grinding, consider using a mouthguard or oral appliance specifically designed to protect the teeth and jaw joint.
Avoid Excessive Strain on the Jaw
Be cautious of habits that place excessive strain on the jaw joint, such as biting hard objects (e.g., pens, nails) or chewing on non-food items. Opt for a balanced and healthy diet that includes foods that are easy to chew.
Maintain Oral Health
Regular dental check-ups can help identify any dental or bite issues that may contribute to TMJ dysfunction. Addressing any dental problems early on can help prevent or minimize the impact on the jaw joint.
It’s important to remember that while these home treatments can provide relief for some individuals, they may not be sufficient for everyone. If your symptoms persist or worsen, it’s advisable to consult with a healthcare professional or dentist specializing in TMJ disorders for a thorough evaluation and appropriate treatment recommendations.
FAQ
Here are some frequently asked questions (FAQ)
How is TMJ Disorder Diagnosed?
TMJ disorder is typically diagnosed through a combination of patient history, physical examination of the jaw joint and muscles, and imaging tests such as X-rays, CT scans, or MRI scans. In some cases, a referral to a dentist or a specialist in TMJ disorders may be necessary for a definitive diagnosis.
Can TMJ Disorder be Treated?
Yes, TMJ disorder can be treated. The treatment approach depends on the severity of symptoms and underlying causes. It may include self-care measures (such as heat or cold therapy, jaw exercises, and stress management), medications, oral appliances (bite guards or splints), physical therapy, and in severe cases, surgical intervention.
Can TMJ Disorder Go Away on its Own?
In some cases, mild TMJ disorder symptoms may improve or resolve on their own with self-care measures and conservative treatments. However, persistent or severe symptoms often require intervention and management to alleviate discomfort and improve jaw function.
Can Stress Worsen TMJ Disorder Symptoms?
Yes, stress and tension can exacerbate TMJ disorder symptoms. Stress can lead to increased clenching or grinding of the teeth, muscle tension, and jaw strain. Managing stress through relaxation techniques, counseling, or stress reduction strategies can help alleviate TMJ symptoms.
Can I Prevent TMJ Disorder?
While it may not be possible to prevent TMJ disorder entirely, certain measures can reduce the risk or minimize the severity of symptoms. This includes maintaining good posture, avoiding excessive jaw movements, practicing stress management techniques, and being mindful of teeth clenching or grinding habits.
How Long Does TMJ Disorder Last?
The duration of TMJ disorder varies from person to person. For some individuals, symptoms may be temporary and resolve within a few weeks or months with self-care measures. However, for others, TMJ disorder can be chronic and persist for a longer period. Seeking proper diagnosis and treatment can help manage symptoms and potentially shorten the duration of the condition.
Can TMJ Disorder Affect Other Parts of the Body?
TMJ disorder primarily affects the jaw joint and surrounding structures, but it can also cause referred pain and symptoms in other areas. It may lead to headaches, neck pain, shoulder pain, and even contribute to ear-related symptoms like earaches or tinnitus (ringing in the ears).
Can TMJ Disorder Cause Dental Problems?
TMJ disorder itself does not cause dental problems, but it can contribute to certain dental issues. Teeth grinding or clenching associated with TMJ disorder can lead to excessive wear on the teeth, tooth sensitivity, and in some cases, jaw muscle fatigue or pain. It’s important to address TMJ dysfunction to minimize its impact on oral health.
Can TMJ Disorder be Related to Sleep Disorders?
TMJ disorder and sleep disorders, such as sleep apnea or bruxism (teeth grinding during sleep), can be interconnected. TMJ disorder can contribute to the development or worsening of sleep disorders, and vice versa. Treating one condition may help alleviate the symptoms of the other.
Can TMJ Disorder be Managed Without Surgery?
Yes, the majority of TMJ disorders can be effectively managed without surgery. Nonsurgical treatments such as self-care measures, medications, oral appliances, physical therapy, and lifestyle modifications are often successful in relieving symptoms and improving jaw function. Surgical intervention is typically considered when conservative approaches have not provided sufficient relief or when there are structural abnormalities requiring surgical correction.
Is TMJ Disorder More Common in Women?
TMJ disorder is more commonly reported in women compared to men. Hormonal factors, such as hormonal changes during menstruation or pregnancy, may contribute to the higher prevalence in women. However, TMJ disorder can occur in individuals of any gender
Can Orthodontic Treatment Help with TMJ Disorder?
Orthodontic treatment, such as braces or other dental interventions, may be beneficial for some individuals with TMJ disorder. Proper alignment of the teeth and bite can help alleviate strain on the jaw joint and improve overall jaw function. It’s important to consult with a dentist or orthodontist experienced in TMJ disorders to determine if orthodontic treatment is appropriate in your specific case.
Conclusion
Temporomandibular joint disorder (TMJ disorder) is a condition that impacts the joint connecting the jawbone to the skull, as well as the muscles in its vicinity. It can cause symptoms such as jaw pain, clicking or popping sounds, limited jaw movement, headaches, and facial pain. The disorder can have various causes, including jaw misalignment, teeth grinding, stress, arthritis, trauma, or hormonal factors. Treatment options range from self-care and lifestyle modifications to medications, oral appliances, physical therapy, and, in severe cases, surgical interventions. While it may not be possible to prevent TMJ disorder entirely, practicing good posture, managing stress, and avoiding excessive jaw movements can help minimize the risk and severity of symptoms. It’s important to consult with healthcare professionals for accurate diagnosis, personalized treatment plans, and guidance on managing TMJ disorder effectively.
Resources
Image Designed by Freepik
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8000442/
https://www.nature.com/articles/s41405-020-0034-8
https://www.frontiersin.org/articles/10.3389/fdmed.2022.1004942/full
https://www.aafp.org/pubs/afp/issues/2015/0315/p378.html
https://www.mdpi.com/2075-4418/11/3/459
https://www.ncbi.nlm.nih.gov/books/NBK551612/
https://www.nidcr.nih.gov/health-info/tmd