We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
What is Tooth Decay?: Tooth decay, also known as dental caries or cavities, is a common oral health problem characterized by the gradual destruction of the tooth structure. The process takes place when the bacteria in your mouth engage with the sugars and starches from food, resulting in the production of acids that harm the enamel, which serves as the tooth’s outer layer Over time, these acids erode the enamel, creating holes or cavities in the tooth. If left untreated, tooth decay can progress to affect the deeper layers of the tooth, leading to pain, infection, and potentially tooth loss.
Table of Contents
ToggleSymptoms of Tooth Decay
The symptoms of tooth decay can vary depending on the severity and location of the decay. Listed below are several typical indications and symptoms:
Toothache
Tooth decay can cause pain or sensitivity in the affected tooth. The pain may be intermittent or constant, and it can range from a dull ache to a sharp, throbbing sensation. The severity of the pain can vary depending on the extent of the cavitie and how close it is to the nerves inside the tooth.
Related: Tooth Pain (Toothache): Overview
Sensitivity
Tooth decay can make the tooth more sensitive to certain stimuli. You may experience heightened sensitivity to hot or cold temperatures, sweet foods or drinks, or acidic substances. When the protective enamel is compromised by decay, these stimuli can reach the underlying dentin or nerve endings, resulting in discomfort or pain.
Visible Pits or Holes
As tooth decay progresses, it can create visible changes on the tooth’s surface. You may notice small pits, holes, or indentations on the affected tooth. These areas can appear as dark spots, stains, or even open cavities. Regular dental examinations and X-rays can help identify these visual signs of decay.
Bad Breath
The bacteria responsible for tooth decay produce acids that break down the tooth structure. These bacteria can also contribute to bad breath. If you notice persistent bad breath, even after practicing good oral hygiene, it could be a sign of tooth caries or other dental issues.
Discoloration
Tooth decay can cause changes in the color of the affected tooth. Initially, there may be white or chalky spots on the enamel, indicating early demineralization. As the decay progresses, the spots can turn yellow, brown, or black. Discoloration can occur on the surface of the tooth or within the cracks and crevices.
Gum Inflammation
When the tooth cavity reaches the gum line or affects the surrounding tissues, it can cause gum inflammation. The gums may appear red, swollen, or tender. In some cases, the gum tissue may even recede, exposing more of the tooth’s surface.
Tooth Sensitivity to Pressure
As tooth caries progresses, the affected tooth can become sensitive to pressure. Biting or applying force on the decayed tooth may cause discomfort or pain. This sensitivity is often an indication that the decay has progressed to deeper layers of the tooth, such as the dentin or pulp, where the nerves are located.
What are the Stages of Tooth Decay?
Tooth decay progresses through several stages, commonly known as the “caries process.” These stages include:
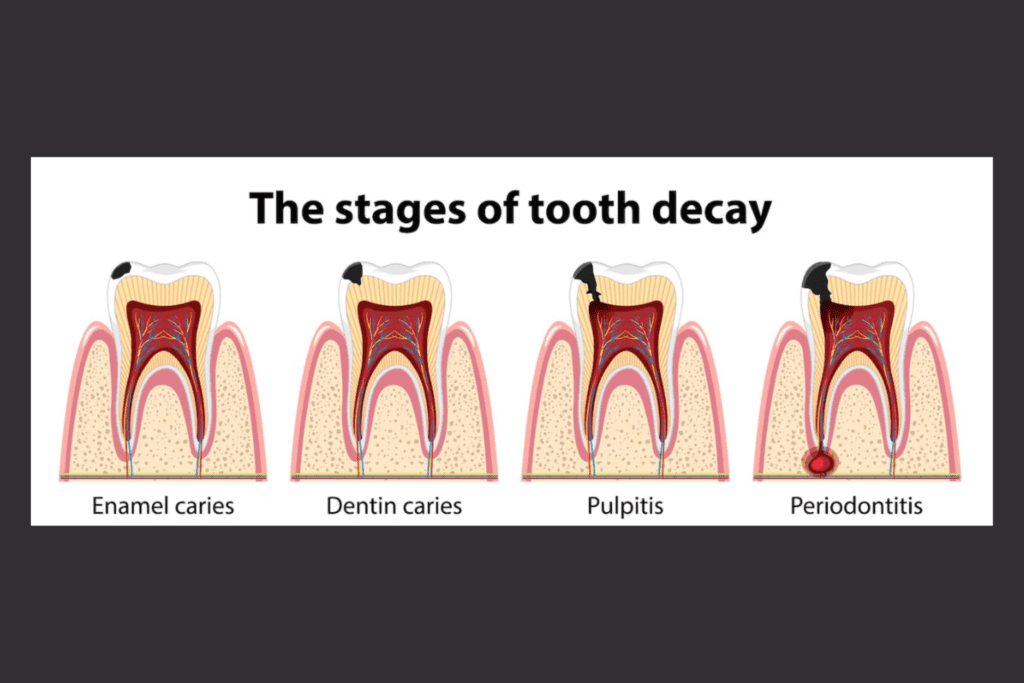
Stage 1: Initial Demineralization
The first stage of tooth caries involves the demineralization of the enamel, which is the outermost protective layer of the tooth. The acid produced by bacteria in the mouth, combined with sugars and starches from food, begins to weaken and break down the enamel. This stage may present as white spots or chalky areas on the tooth surface.
Stage 2: Enamel Decay
As the demineralization continues, the enamel begins to break down, resulting in the formation of a cavity or hole in the tooth. At this stage, the decay is still limited to the outer layer of the tooth and may not cause any symptoms or pain.
Stage 3: Dentin Decay
If the decay progresses beyond the enamel, it reaches the dentin, which is the softer layer beneath the enamel. Dentin is more vulnerable to acid attacks, and the decay can spread more rapidly. At this stage, the decay may cause increased tooth sensitivity, especially to hot, cold, sweet, or acidic substances.
Stage 4: Pulp Involvement
When the decay reaches the innermost layer of the tooth, called the pulp, it can cause significant damage and discomfort. Within the pulp reside nerves, blood vessels, and connective tissue. Involvement of the pulp often leads to intense toothache, increased sensitivity, swelling, and potential infection. Treatment at this stage may require root canal therapy or, in severe cases, tooth extraction.
Stage 5: Abscess Formation
In the advanced stage of tooth decay, an abscess may form at the root of the affected tooth. An abscess forms as a result of a bacterial infection, leading to the accumulation of pus. It can cause intense pain, swelling, and systemic symptoms such as fever and malaise. Prompt dental intervention is necessary to treat the infection and prevent further complications.
Related: Tooth Abscess
What are the Causes of Tooth decay or Cavity?
Tooth decay, also known as dental caries or cavities, is primarily caused by a combination of factors that promote the growth and activity of harmful bacteria in the mouth. Primary factors contributing to tooth decay comprise:
Poor Oral Hygiene
Inadequate oral hygiene practices, such as irregular brushing and improper flossing, can lead to the buildup of plaque on the teeth. Plaque refers to a sticky film consisting of bacteria, food particles, and saliva. If not removed regularly, plaque can contribute to tooth caries.
Bacterial Activity
The mouth naturally contains various types of bacteria, including Streptococcus mutans and Lactobacillus, which are known to produce acids that attack tooth enamel. These bacteria feed on sugars and carbohydrates from food and beverages, converting them into acids that erode the tooth structure over time.
Sugary and Acidic Foods
Consuming a diet high in sugary foods and drinks, such as candies, sodas, and sugary snacks, provides an abundant food source for the bacteria in the mouth. Additionally, consuming acidic foods and beverages, like citrus fruits and carbonated drinks, can directly contribute to enamel erosion and tooth caries.
Dry Mouth (Xerostomia)
Saliva plays a vital role in maintaining oral health by neutralizing acids and washing away food particles and bacteria. A dry mouth condition, often caused by certain medications, medical conditions, or mouth breathing, reduces saliva flow and increases the risk of tooth decay.
Tooth Anatomy
The structure and alignment of teeth can affect the risk of tooth decay. Deep grooves and pits on the chewing surfaces of teeth can trap bacteria and make them harder to clean. Similarly, crowded or misaligned teeth can create tight spaces where plaque and bacteria can accumulate.
Lack of Fluoride
Fluoride is a mineral that helps strengthen tooth enamel and makes it more resistant to acid attacks. Insufficient exposure to fluoride, whether through fluoridated water, toothpaste, or professional treatments, can increase the susceptibility to tooth decay.
Age and Genetics
Children and older adults are more prone to tooth decay. Children may have less developed oral hygiene habits, while older adults may have receding gums or decreased saliva production. Genetics also play a role in tooth decay susceptibility, with some individuals being more prone to cavities due to inherited factors.
Does Mouth pH Affect Tooth Decay?
Yes, the pH level in the mouth can affect tooth decay. The pH scale measures the acidity or alkalinity of a substance, with values ranging from 0 to 14. A pH level of 7 is deemed neutral, whereas values below 7 indicate acidity and values above 7 indicate alkalinity.
When the mouth’s pH is below 5.5, it becomes acidic, which can contribute to tooth decay. The acidic environment promotes the demineralization of tooth enamel, the outer protective layer of the tooth, making it more susceptible to decay.
The acidity in the mouth is influenced by various factors, including the types of foods and drinks consumed. Foods and beverages are high in sugars and carbohydrates, especially those that are sticky or consumed frequently throughout the day can create an acidic environment in the mouth. This is because bacteria in the mouth feed on these sugars and produce acids as byproducts, which attack the tooth enamel.
Additionally, certain medical conditions, such as acid reflux or dry mouth (xerostomia), can affect the pH in the mouth and increase the risk of tooth decay. Acid reflux introduces stomach acids into the mouth, while dry mouth reduces saliva flow, which usually helps neutralize acids and wash away food particles.
Maintaining a balanced pH in the mouth is crucial for oral health. To minimize the risk of tooth decay, it’s important to practice good oral hygiene, limit the consumption of sugary and acidic foods and drinks, and drink plenty of water to help maintain a neutral pH in the mouth.
Diagnosis of Tooth Decay
The diagnosis of tooth caries is typically performed by a dentist during a dental examination. Here are the common methods and techniques used for diagnosing tooth decay:
Visual Examination
The dentist will visually inspect your teeth, looking for visible signs of decay such as discoloration, white spots, or visible cavities. They will also check for any abnormalities in the tooth structure or signs of erosion.
Dental Probing
Using a dental probe, the dentist gently explores the surfaces of your teeth to check for soft or sticky areas that may indicate tooth decay. They will pay close attention to the areas where decay commonly occurs, such as the biting surfaces, grooves, and the spaces between teeth.
Dental X-rays
X-rays, also known as dental radiographs, are commonly used to detect tooth caries that may not be visible during a visual examination. X-rays can reveal decay between the teeth or beneath existing dental restorations. They provide a more detailed view of the teeth, allowing the dentist to assess the extent of the decay and determine the most appropriate treatment.
Laser Fluorescence Cavity Detection
Some dentists may use a special laser device to detect early-stage tooth cavities. The laser emits light onto the tooth surface, and based on the fluorescence patterns, the dentist can assess the presence and severity of the decay.
Dye or Stain
In certain cases, the dentist may apply a dye or stain to the teeth. The dye adheres to areas of decay, making them more visible during the examination.
Electrical Conductivity Measurement
Advanced diagnostic tools, such as electrical conductivity devices, may be used to measure changes in the electrical conductivity of the tooth structure. These changes can indicate the presence of decay.
What is the Treatment Option for Tooth Decay?
There are several treatment options for tooth decay, depending on the severity and extent of the cavity. Here are some common treatment options:
Dental Fillings
If the decay is limited to a small area, the dentist removes the decayed portion of the tooth and fills the cavity with a dental filling material such as composite resin, amalgam, or glass ionomer cement.
Dental Crowns
If the decay is extensive and has weakened the tooth, a dental crown may be recommended. The decayed portion is removed, and a custom-made crown is placed over the remaining tooth structure to restore its shape, strength, and function.
Root Canal Treatment

When tooth decay reaches the innermost part of the tooth called the pulp, a root canal treatment may be necessary. During a root canal treatment, the dentist eliminates the infected pulp, thoroughly cleans and disinfects the root canals, and subsequently fills and seals them to ensure proper healing and protection. A crown is typically placed on the tooth to protect and strengthen it.
Dental Inlays and Onlays
These are indirect restorations used when the decayed area is too large for a filling but doesn’t require a full crown. Inlays are placed within the tooth’s cusps, while onlays cover one or more cusps.
Tooth Extraction
In cases where the tooth is severely decayed and cannot be restored, extraction may be necessary. After extraction, options for tooth replacement, such as dental implants, bridges, or dentures, can be considered.
How to Prevent Tooth Decay?
Maintaining good oral health necessitates the prevention of tooth decay. Here are some effective strategies to help prevent tooth decay:
Maintain Proper Oral Hygiene
Brush your teeth at least twice a day using fluoride toothpaste, employing a soft-bristle toothbrush and gentle circular motions to thoroughly clean all tooth surfaces and the gum line. Remember to include tongue brushing in your oral hygiene routine. Moreover, develop a daily flossing habit to effectively eliminate plaque and food particles from the spaces between your teeth and along the gum line.
Use Fluoride Toothpaste and Mouthwash
Fluoride strengthens tooth enamel and helps protect against decay. Choose a toothpaste and mouthwash that contain fluoride to provide extra protection for your teeth.
Limit Sugary and Acidic Foods and Drinks
Reduce your consumption of sugary foods and beverages, such as candies, sodas, cakes, and cookies. When you do consume them, try to do so during meals rather than as snacks. Also, minimize your intake of acidic foods and drinks like citrus fruits, juices, and carbonated beverages, as they can erode tooth enamel.
Drink Water and Rinse After Meals
Drinking water after meals helps rinse away food particles and neutralize the acid in the mouth. Swishing water around your mouth after eating can help remove debris and promote saliva production, which aids in demineralizing and protecting the teeth.
Maintain a Balanced Diet
Eating a balanced diet that includes a variety of fruits, vegetables, whole grains, and lean proteins supports overall oral health. Include foods rich in calcium, such as dairy products and leafy greens, as they contribute to strong teeth and bones.
Chew Sugar-Free Gum
Chewing sugar-free gum, especially after meals, stimulates saliva flow. Saliva helps wash away food particles, neutralize acids, and demineralize tooth enamel. Look for gum with the ADA (American Dental Association) seal of approval.
Drink Fluoridated Water
If your tap water is fluoridated, drink it regularly as it provides a natural source of fluoride. Fluoridated water helps strengthen tooth enamel and protect against tooth decay.
Visit the Dentist Regularly
Ensure that you schedule regular dental check-ups and professional cleanings as part of your routine. Dentists can detect early signs of decay, provide preventive treatments (like fluoride applications and dental sealants), and address any oral health concerns promptly.
Consider Dental Sealants
Dental Sealants are thin plastic coatings that are carefully applied to the chewing surfaces of the molars and premolars, which are located at the back of the mouth. They act as a protective barrier against plaque and acid attacks, reducing the risk of decay in these susceptible areas.
Teach and Practice Good Oral Hygiene Habits
Educate children and family members about the importance of proper oral hygiene. Encourage regular brushing, flossing, and the use of fluoride products to instill lifelong habits.
By implementing these preventive measures and maintaining a consistent oral care routine, you can significantly reduce the risk of tooth caries and promote long-term oral health.
Conclusion
In conclusion, tooth decay, also known as dental caries or cavities, is a common oral health problem caused by bacteria, sugars, and poor oral hygiene. It can lead to various symptoms, such as tooth sensitivity, pain, and visible damage to the teeth. Tooth decay progresses through different stages, starting with the formation of a white spot lesion and eventually leading to extensive damage and tooth loss if left untreated.
Diagnosing tooth decay involves a combination of visual examination, dental probing, dental X-rays, and advanced diagnostic tools. Early detection is crucial for effective treatment and preventing further complications. The treatment options for tooth decay depend on the severity and extent of the decay. They can range from fluoride treatments and dental fillings for early-stage decay to more invasive procedures like root canal treatment or tooth extraction for advanced decay.
Tooth decay is primarily prevented through proper oral hygiene practices, including regular brushing and flossing, using fluoride toothpaste and mouthwash, and limiting the consumption of sugary and acidic foods and drinks. Maintaining a balanced diet, drinking fluoridated water, visiting the dentist regularly, and considering preventive measures like dental sealants also play a vital role in preventing tooth decay.
It’s important to consult a dentist for a proper diagnosis and appropriate treatment. By implementing preventive measures and practicing good oral hygiene, individuals can significantly reduce the risk of tooth decay and maintain optimal oral health. Regular dental check-ups, early intervention, and a proactive approach are key to preventing and managing tooth decay effectively.
Read next: Tooth Infection Symptoms
Resources
Image Designed by freepik
Reference
https://www.mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892?p=1
https://www.nidcr.nih.gov/health-info/tooth-decay
https://medlineplus.gov/lab-tests/dental-exam/
https://www.nidcr.nih.gov/health-info/fluoride
https://www.nidcr.nih.gov/health-info/dental-fillings
https://www.nidcr.nih.gov/health-info/dental-sealants
https://www.merckmanuals.com/home/mouth-and-dental-disorders/tooth-disorders/cavities
https://www.webmd.com/oral-health/what-to-know-tooth-decay-stages





