We sometimes add products that we believe may be beneficial to our readers. We may receive a small commission if you purchase using the links on this page. Read our affiliate disclaimer
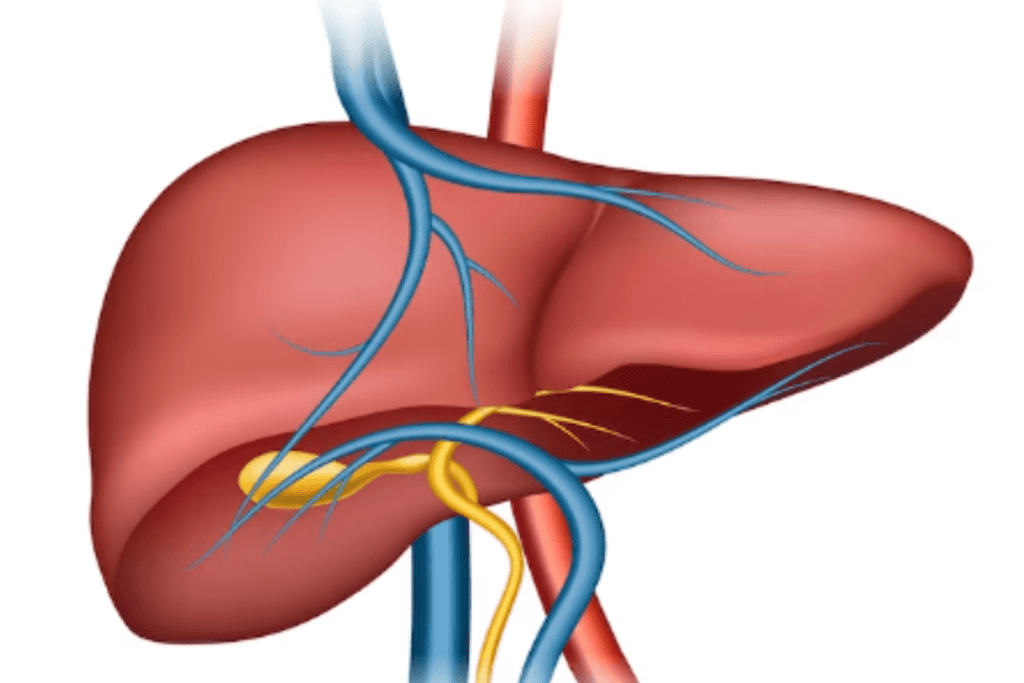
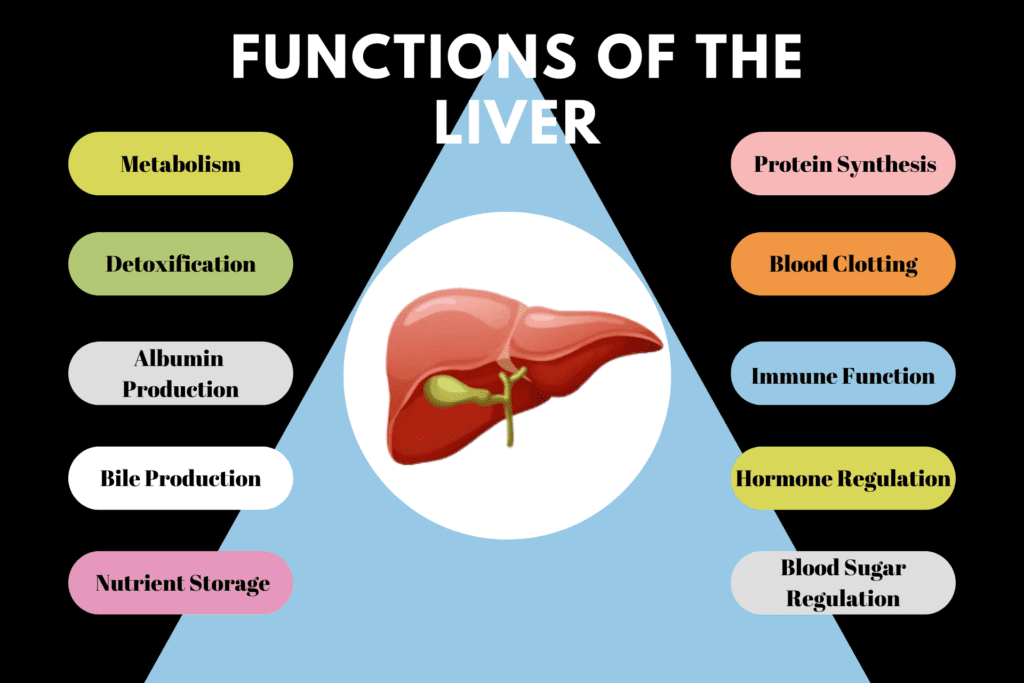
10 Functions of the Liver: The liver, a remarkable organ, plays a pivotal role in maintaining the body’s homeostasis and overall well-being. From metabolism and detoxification to nutrient storage, hormone regulation, and blood sugar control, the liver performs a wide array of vital functions. It processes nutrients, detoxifies harmful substances, and synthesizes proteins critical for immune function. The liver’s role in hormone metabolism ensures hormonal balance, while its ability to store and release glucose helps regulate blood sugar levels.
Table of Contents
ToggleThe liver performs several important functions that are crucial for maintaining overall health. Here are 10 of the most important liver functions:
1. Metabolism
Metabolism is the set of biochemical processes that occur within an organism to maintain life. The liver plays a crucial role in metabolism and is responsible for processing various nutrients, including carbohydrates, proteins, and fats. Let’s delve into the liver’s role in metabolizing these nutrients:
Carbohydrate Metabolism
When we consume carbohydrates, they are broken down into glucose, a simple sugar that serves as the primary source of energy for our body. After a meal, blood glucose levels rise, and to prevent excessive glucose buildup, the liver steps in to regulate this process.
Glycogenesis
The liver converts excess glucose into glycogen, a branched chain of glucose molecules, and stores it. This stored glycogen acts as a reservoir of glucose that can be broken down and released back into the bloodstream when the body needs additional energy, such as during periods of fasting or physical activity.
Glycogenolysis
When the body requires energy, hormones like glucagon signal the liver to break down glycogen into glucose through a process called glycogenolysis. This glucose is then released into the bloodstream to fuel various tissues and organs.
Protein Metabolism
When we consume proteins in our diet, they are broken down into their constituent amino acids during digestion. The liver is responsible for processing these amino acids and carrying out various functions related to protein metabolism
Protein Synthesis
The liver synthesizes specific proteins, such as albumin and blood clotting factors, that are essential for various physiological processes in the body. These proteins are released into the bloodstream to perform their respective functions.
Deamination
Excess amino acids that are not required for protein synthesis are deaminated in the liver. This process involves removing the amino group from the amino acid, converting it into ammonia. The liver then further processes the ammonia, converting it into urea, which is eventually eliminated through urine.
Fat metabolism
The liver also plays a key role in processing dietary fats and maintaining lipid balance in the body.
Lipogenesis
When there is an excess of glucose or amino acids, the liver can convert them into fatty acids, which are then combined with glycerol to form triglycerides. These triglycerides are stored in adipose tissue for long-term energy storage.
Lipolysis
In times of energy need, the liver can break down stored triglycerides in adipose tissue and release fatty acids into the bloodstream to be used as an energy source.
Cholesterol synthesis
The liver synthesizes cholesterol, which is essential for various functions in the body, such as hormone production and cell membrane formation.
2. Detoxification
Indeed, the liver plays a vital role in detoxification, which involves the processing and removal of harmful substances, toxins, drugs, alcohol, metabolic waste products, and environmental pollutants from the body. This detoxification process occurs primarily in hepatocytes, the functional cells of the liver, and involves several biochemical pathways.
Let’s explore how the liver carries out detoxification:
Phase I Detoxification
In this phase, the liver converts the toxic substances into intermediate metabolites, making them more water-soluble and easier to eliminate. This step is primarily achieved through enzymatic reactions, mainly mediated by the cytochrome P450 (CYP450) enzyme system.
Oxidation:
The CYP450 enzymes add oxygen molecules to the toxic compounds, making them more reactive and introducing functional groups that can be targeted in the next phase of detoxification.
Reduction:
Some substances are reduced by enzymes, which add electrons to the toxic compounds and reduce their reactivity.
Hydrolysis:
Hydrolytic enzymes break down certain toxic substances into smaller, less harmful components.
Phase II Detoxification
During this phase, the liver modifies the intermediate metabolites produced in Phase I detoxification to increase their water solubility significantly. This enhances the ability to eliminate them from the body effectively. Phase II detoxification involves conjugation reactions, where the liver adds specific molecules to the intermediate metabolites.
Glucuronidation:
One of the most common conjugation reactions in the liver is glucuronidation. In this process, glucuronic acid is added to the intermediate metabolites, forming glucuronides. These glucuronides are highly water-soluble and easily excreted in the bile or urine.
Sulfation:
Sulfate molecules are added to the intermediate metabolites, creating sulfates, which are also highly water-soluble and easily eliminated.
Glutathione Conjugation:
Glutathione, a powerful antioxidant present in the liver, binds to and neutralizes many harmful substances and is critical for the detoxification of certain drugs and environmental pollutants.
Bile Secretion and Elimination:
After Phase II detoxification, the water-soluble and conjugated metabolites are transported into bile canaliculi, small ducts within the liver. These canaliculi eventually merge to form the common bile duct, through which the bile flows into the gallbladder for storage. When needed, the gallbladder releases bile into the small intestine, where some of the toxins and waste products are eliminated in the feces.
Urinary Elimination:
Water-soluble metabolites produced during detoxification can be filtered by the kidneys and eliminated through urine.
3. Albumin Production
Albumin production is indeed a vital function of the liver. Albumin is the most abundant protein in blood plasma, and it plays a crucial role in maintaining various physiological processes.
The liver is responsible for synthesizing albumin and secreting it into the bloodstream. Once in circulation, albumin serves several essential functions:
Fluid Balance
Albumin helps regulate the distribution of fluids between the blood vessels and surrounding tissues. It creates osmotic pressure, which prevents excessive fluid from leaking out of blood vessels into the tissues, maintaining fluid balance and preventing edema (swelling).
Transport
Albumin acts as a carrier protein, transporting various substances in the bloodstream. It binds to and carries hormones, fatty acids, bilirubin (a waste product of red blood cell breakdown), and certain medications, facilitating their transport to different parts of the body.
pH Regulation
Albumin acts as a buffer in the blood, helping to stabilize and regulate the blood’s pH level. It can bind to and release hydrogen ions, contributing to the body’s acid-base balance.
Immune Support
Albumin is involved in the body’s immune response. It can bind to and transport certain hormones and compounds related to the immune system, supporting immune function.
Wound Healing
Albumin plays a role in the wound-healing process by transporting nutrients and other essential molecules to the injured tissues, aiding in tissue repair.
4. Bile Production
Bile production is a crucial function of the liver, and bile plays a critical role in the digestion and absorption of fats in the digestive system. Bile is a greenish-yellow fluid composed of bile salts, cholesterol, bilirubin, phospholipids, water, and electrolytes. It is produced in the liver and then stored and concentrated in the gallbladder until needed.
The process of bile production and its role in fat digestion can be explained as follows:
Bile Production
The liver continuously produces bile, which is a complex mixture of substances. The liver cells, known as hepatocytes, synthesize bile salts from cholesterol, which are essential for the digestion and absorption of fats.
Bile Secretion
The bile produced by the liver is secreted into small bile ducts, which merge to form larger bile ducts. These bile ducts eventually combine to form the common hepatic duct, which transports bile away from the liver.
Bile Storage
Bile flows through the common hepatic duct and enters the gallbladder, a small, pear-shaped organ located beneath the liver. The gallbladder acts as a storage reservoir for bile, where it is concentrated and stored between meals.
Bile Release
When we consume a meal containing fats, the gallbladder contracts and releases bile through the common bile duct into the small intestine. Bile is released in response to the hormone cholecystokinin, which is produced in response to the presence of fats in the small intestine.
Role in Fat Digestion
Bile salts in the bile play a crucial role in fat digestion. They emulsify the large fat globules into smaller droplets, increasing the surface area of fats and making them more accessible to digestive enzymes called lipases. Lipases can then break down the smaller fat droplets into fatty acids and monoglycerides, which are easier to absorb.
Absorption of Fats
The smaller fatty acids and monoglycerides formed by the action of lipases can be absorbed across the intestinal lining into the bloodstream and transported to various tissues for energy production and other physiological processes.
After aiding in the digestion and absorption of fats, bile is eventually reabsorbed and recycled back to the liver for further use.
5. Nutrient Storage
Indeed, the liver plays a significant role in nutrient storage, acting as a reservoir for various essential vitamins and minerals. These stored nutrients are critical for supporting various metabolic processes in the body. Let’s explore how the liver stores and releases these nutrients:
Fat-Soluble Vitamins (A, D, E, K)
The liver stores fat-soluble vitamins, which are vitamins that dissolve in fats. These vitamins are absorbed from the diet and are not water-soluble like most other vitamins. The liver accumulates excess fat-soluble vitamins and stores them in specialized cells called hepatic stellate cells or in the liver tissue itself. When the body requires these vitamins for metabolic processes, the liver releases them into the bloodstream, ensuring a steady supply for various functions, including immune support (vitamin A), bone health (vitamin D), antioxidant protection (vitamin E), and blood clotting (vitamin K).
Water-Soluble Vitamins (B12)
While most water-soluble vitamins, like vitamin C and B-complex vitamins, are not significantly stored in large amounts in the liver, vitamin B12 is an exception. The liver can store a significant amount of vitamin B12, primarily in the form of methylcobalamin. Vitamin B12 is essential for nerve function, red blood cell production, and DNA synthesis. The liver stores B12 in high concentrations, and when the body needs it, the liver releases this vitamin into the bloodstream, ensuring a continuous supply for vital physiological processes.
Minerals (Iron and Copper)
The liver also serves as a storage site for certain minerals, particularly iron and copper. Iron is stored in the liver primarily in the form of ferritin, a protein complex that can bind to iron ions. The liver regulates the release of iron into the bloodstream, ensuring a controlled and balanced supply to meet the body’s needs for hemoglobin production and various enzymatic functions. Similarly, the liver stores copper, which is a crucial trace element involved in various enzymatic reactions, and releases it into the bloodstream as needed.
6. Protein Synthesis
Protein synthesis is a crucial function of the liver, and it produces a diverse array of proteins that are essential for maintaining various physiological processes. The liver’s involvement in protein synthesis can be explained as follows:
Albumin
As mentioned earlier, albumin is the most abundant protein in the blood plasma, and it is synthesized by the liver. Albumin plays a critical role in maintaining proper fluid balance by exerting osmotic pressure, preventing excessive fluid from leaking out of blood vessels into the surrounding tissues. This helps to regulate the distribution of fluids in the body and prevent edema (swelling).
Clotting Factors
The liver is responsible for synthesizing several clotting factors, which are essential for blood coagulation. Clotting factors play a crucial role in the formation of blood clots, which is vital to prevent excessive bleeding and promote wound healing.
Immune Proteins
The liver produces various immune proteins, including complement proteins and acute-phase reactants. Complement proteins are part of the immune system’s defense mechanism against pathogens, aiding in the destruction of foreign invaders. Acute-phase reactants are proteins that increase in concentration during inflammation or infection, helping to modulate the immune response and promote tissue repair.
Transport Proteins
The liver synthesizes numerous transport proteins that aid in the transport of various substances in the blood. For example, as mentioned earlier, albumin is a carrier protein that transports hormones, fatty acids, bilirubin, and medications. Additionally, the liver produces lipoproteins that transport lipids, such as cholesterol and triglycerides, into the bloodstream.
7. Blood Clotting
Blood clotting, also known as coagulation, is a complex and essential process that prevents excessive bleeding when there is an injury or damage to blood vessels. The liver plays a crucial role in blood clotting by producing various clotting factors, including fibrinogen and prothrombin, which are necessary for the proper formation of blood clots. Here’s an explanation of how the liver’s clotting factors work:
Formation of Platelet Plug
When a blood vessel is injured, platelets in the bloodstream are activated and rush to the site of injury. They adhere to the damaged vessel wall and aggregate together to form a temporary plug, sealing the wound.
Activation of Clotting Factors
Upon vessel injury, the liver releases clotting factors into the bloodstream. Fibrinogen, also known as Factor I, is a soluble plasma protein present in the blood. Prothrombin, also known as Factor II, is an inactive precursor of thrombin, an enzyme responsible for the final step of blood clot formation.
Conversion of Prothrombin to Thrombin
The clotting factors released by the liver activate a series of enzymatic reactions known as the coagulation cascade. One of the critical steps in this cascade is the conversion of prothrombin to thrombin, which occurs in the presence of calcium ions and certain other clotting factors.
Fibrin Formation
Thrombin acts on fibrinogen, cleaving it into smaller fragments. These fragments, called fibrin monomers, spontaneously assemble into a mesh-like network called fibrin. Fibrin forms the structural framework of the blood clot.
Blood Clot Formation
The fibrin mesh, along with the platelet plug, consolidates to form a stable blood clot. The clot acts as a physical barrier, preventing further blood loss from the injured site.
Clot Retraction and Dissolution
After the wound has healed, the clot undergoes a process called clot retraction, where it becomes more compact. As the injured tissue heals, the clot eventually dissolves through a process called fibrinolysis, which involves the breakdown of fibrin by plasmin, an enzyme that maintains blood fluidity.
8. Immune Function
The liver’s immune function is closely tied to the presence of specialized immune cells called Kupffer cells. Kupffer cells are a type of macrophage, which are large phagocytic cells responsible for engulfing and destroying foreign particles, bacteria, viruses, and cellular debris. The liver contains a high concentration of Kupffer cells, making it a significant component of the body’s immune defense system. Here’s an explanation of how Kupffer cells contribute to the liver’s immune function:
Phagocytosis
Kupffer cells actively patrol the liver sinusoids, which are small blood vessels in the liver. They recognize and engulf foreign particles, such as bacteria, viruses, and damaged cells, through a process called phagocytosis. By removing these harmful substances from the bloodstream, Kupffer cells play a critical role in protecting the liver from infections.
Antigen Presentation
When Kupffer cells encounter foreign substances, they process and present specific components of these substances, called antigens, to other immune cells, such as T cells. This process is crucial for initiating a targeted and specific immune response against invading pathogens.
Modulation of Immune Response
Kupffer cells can also secrete various signaling molecules, called cytokines, that regulate the immune response. Depending on the situation, these cytokines can either stimulate or dampen immune activity. By modulating the immune response, Kupffer cells help maintain immune homeostasis and prevent excessive inflammation.
Liver Infections and Immune Defense
The liver is an essential site for immune defense, especially against infections that may enter the bloodstream through the digestive system. Kupffer cells play a key role in detecting and eliminating pathogens, preventing them from spreading and causing widespread infection.
Tolerance and Immune Regulation
Beyond their role in fighting infections, Kupffer cells also play a part in maintaining immune tolerance. They help regulate the immune response to prevent the body from mounting an excessive immune attack against its tissues.
9. Hormone Regulation
Indeed, the liver is involved in hormone regulation through its role in hormone metabolism. This function is vital for maintaining hormonal homeostasis, ensuring that hormones are appropriately metabolized and eliminated from the body to prevent hormonal imbalances.
Here’s an explanation of how the liver contributes to hormone regulation:
Hormone Metabolism
Various hormones circulate in the bloodstream, and their levels need to be tightly regulated to ensure proper physiological functioning. The liver plays a significant role in metabolizing hormones that have completed their respective functions in the body. As hormones travel through the bloodstream, they eventually reach the liver, where they undergo metabolic transformations.
Inactivation and Clearance
The liver acts as a filter, inactivating and clearing hormones that are no longer needed or have fulfilled their roles. Specific enzymes in the liver, such as UDP-glucuronosyltransferases and sulfotransferases, facilitate the conjugation of hormones with molecules like glucuronic acid or sulfate. This process makes the hormones more water-soluble and facilitates their excretion from the body.
Hormonal Balance
By metabolizing and eliminating hormones, the liver helps maintain hormonal balance in the body. Hormonal imbalances can lead to various health issues, such as endocrine disorders, reproductive problems, and metabolic disturbances. Proper hormone regulation is essential for overall health and well-being.
Influence on Hormone Levels
The liver’s ability to metabolize and clear hormones can affect its circulating levels in the bloodstream. For example, impaired liver function may result in reduced hormone clearance, leading to elevated hormone levels. Conversely, a well-functioning liver efficiently removes excess hormones, preventing hormone buildup and potential adverse effects.
Impact on Drug Metabolism
The liver’s role in hormone metabolism can also influence the metabolism of certain medications and drugs. Some medications are metabolized by the same liver enzymes responsible for hormone metabolism, leading to potential drug-hormone interactions.
10. Blood Sugar Regulation
The liver plays a crucial role in blood sugar regulation through its ability to store and release glucose in the form of glycogen. This process helps maintain stable blood sugar levels and prevents both hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar).
Here’s an explanation of how the liver contributes to blood sugar regulation:
Glycogenesis (Storage of Glucose as Glycogen)
When blood sugar levels are high, such as after a meal, excess glucose is taken up by various tissues in the body, including the liver. The liver converts this excess glucose into glycogen through a process called glycogenesis. Glycogen is a polysaccharide that serves as a storage form of glucose.
Glycogenolysis (Release of Glucose from Glycogen)
When blood sugar levels begin to drop, the body requires a constant supply of glucose to maintain normal bodily functions and energy production. In response to signals, such as low blood sugar or hormones like glucagon, the liver initiates glycogenolysis. This process involves breaking down glycogen into individual glucose molecules and releasing them into the bloodstream.
Gluconeogenesis (Production of Glucose from Non-Carbohydrate Sources)
In addition to glycogenolysis, the liver can also produce glucose from non-carbohydrate sources, such as amino acids (building blocks of proteins) and glycerol (derived from fats). This process, called gluconeogenesis, is another mechanism that the liver uses to maintain blood sugar levels during prolonged fasting or when glucose intake is insufficient.
Insulin and Glucagon Regulation
Blood sugar levels are tightly regulated by the balance between two hormones: insulin and glucagon. After a meal, when blood sugar levels rise, the pancreas releases insulin, which promotes glucose uptake by cells and storage of excess glucose as glycogen in the liver. Conversely, during periods of fasting or low blood sugar, the pancreas releases glucagon, which stimulates glycogenolysis and gluconeogenesis in the liver, leading to the release of glucose into the bloodstream.
Conclusion
In conclusion, the liver is a remarkably versatile and vital organ that performs numerous essential functions crucial for overall health and well-being. From metabolism to detoxification, nutrient storage, hormone regulation, and blood sugar control, the liver plays a central role in maintaining homeostasis within the body.
Through its metabolic activities, the liver processes and stores carbohydrates, proteins, and fats, providing energy and essential nutrients as needed. It detoxifies harmful substances and facilitates their elimination from the body, safeguarding against potential damage. Additionally, the liver supports immune function by housing Kupffer cells that filter and remove pathogens from the bloodstream, protecting against infections.
The liver also contributes to hormonal balance and blood sugar regulation, acting as a storage site for essential vitamins, minerals, and hormones. Its ability to release stored glycogen as glucose helps maintain stable blood sugar levels, preventing hypoglycemia and hyperglycemia.
Overall, the liver’s multifaceted functions underscore its significance as a crucial organ responsible for supporting numerous vital processes, making its health and proper functioning imperative for overall wellness.
References
https://www.ncbi.nlm.nih.gov/books/NBK535438/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4050641/
https://pubmed.ncbi.nlm.nih.gov/1749210/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681351/